The research information about using atropine to manage myopia progression is constantly evolving. To understand what is currently being applied in clinical practice more, PC created an interesting poll about atropine usage on the Myopia Profile Facebook discussion group. Note this poll was taken in October 2019.
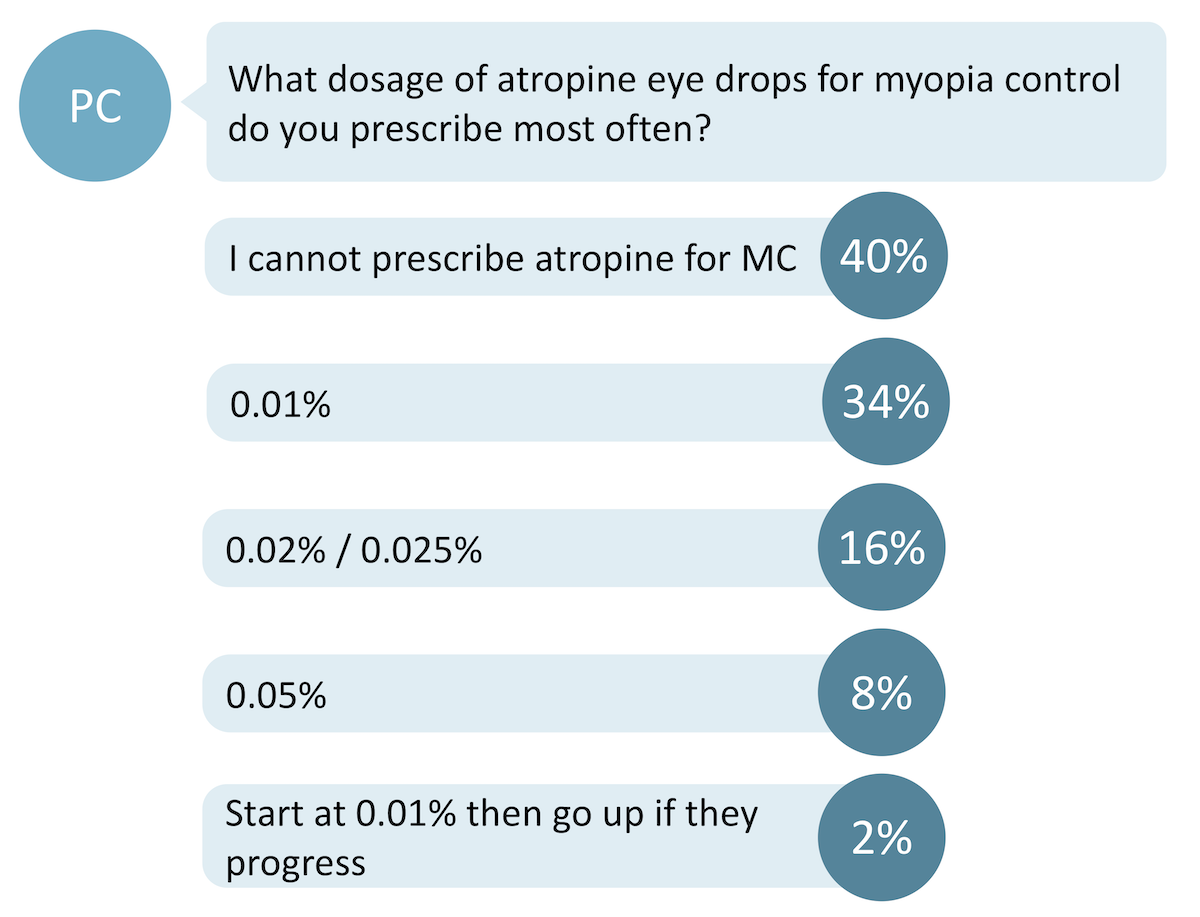
Out of 244 voters, 40% responded that they could not prescribe atropine for myopia control – likely due to scope of primary eye care practice in their country. Of the primary eye care professions, only appropriately trained optometrists in the US, Australia and New Zealand can prescribe atropine at this stage. All ophthalmologists can prescribe atropine.
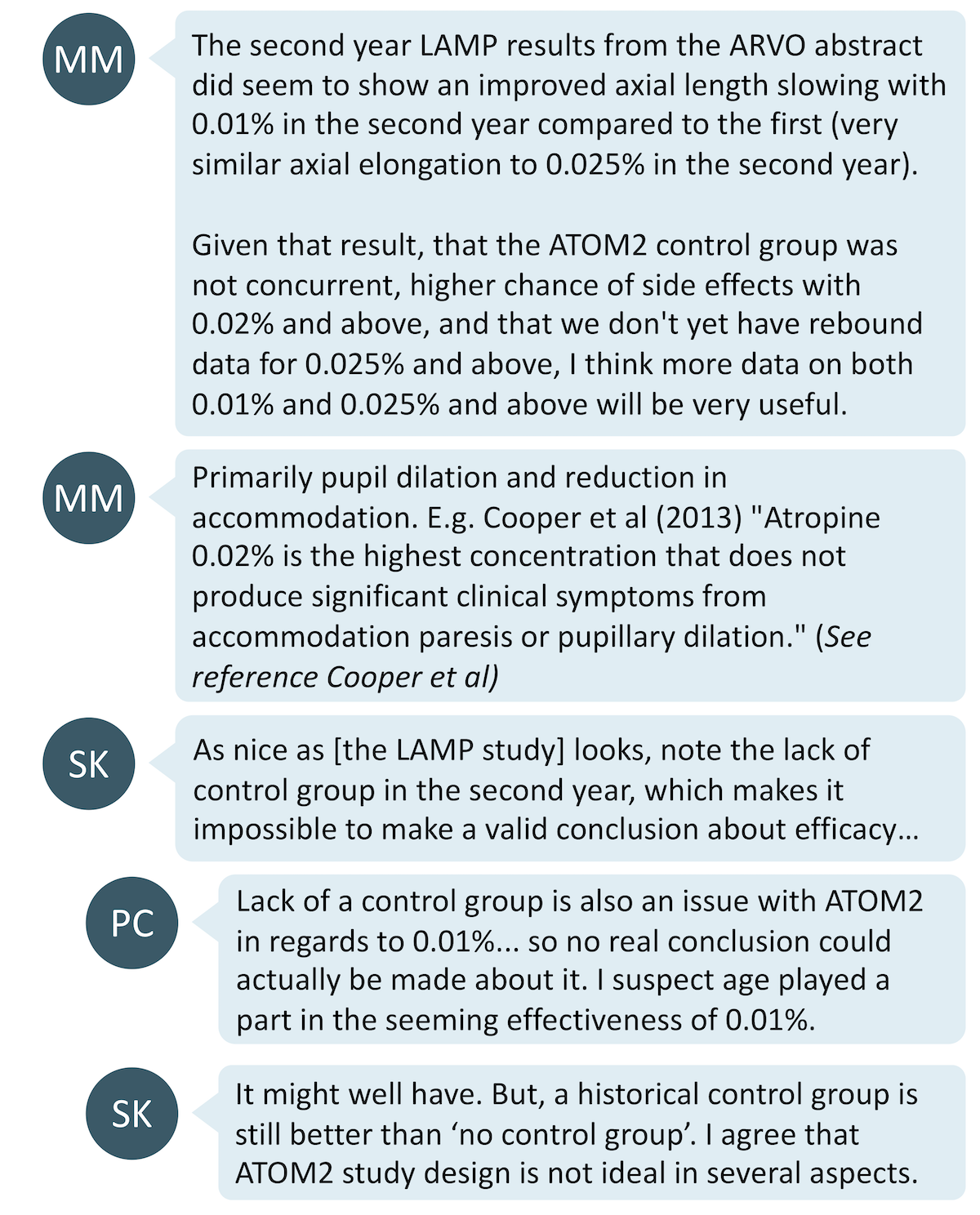
Of those who do prescribe atropine eye drops for myopia control, the majority of this group either use only 0.01% or start with 0.01% with the intention to increase the concentration over time or depending on myopia progression. The remainder of the respondents use higher concentrations. Here is what the community said on the topic.
The suitability of 0.01% atropine has split the community
This poll showed us that a large proportion of practitioners still prescribe atropine at the 0.01% concentration.
1. Some have had great success with 0.01%
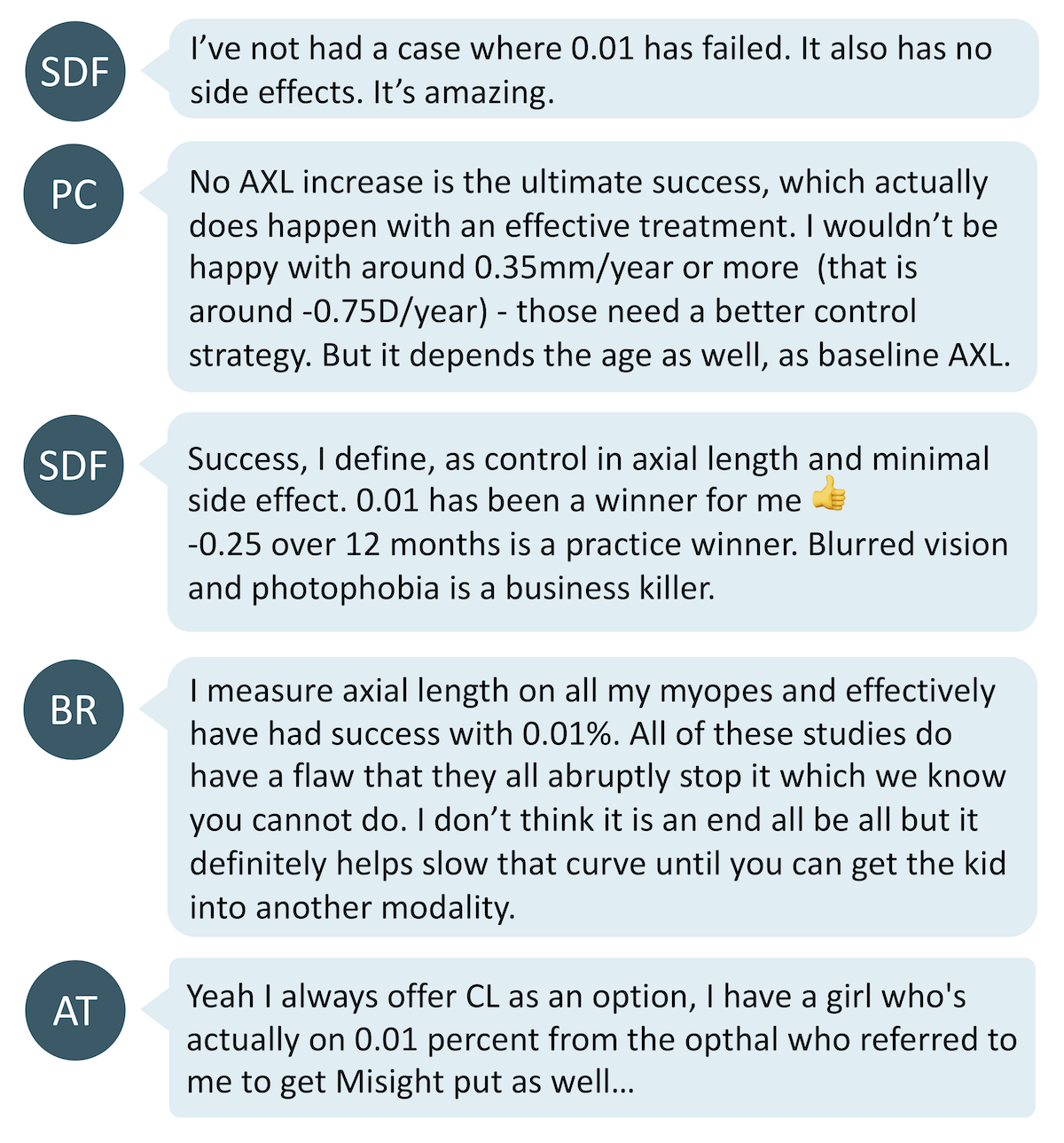
It is interesting that practitioners mention patient tolerance and minimal side effects as a key factor of treatment success; and also how studies which abruptly halt treatments do not reflect typical clinical care.
Prescribing 0.01% as a monotherapy, though, appears to be at odds with the findings of the LAMP study1, whereby 0.01% was found to be ineffective for controlling axial length elongation. Perhaps there are additional differences in clinical practice that contribute to the anecdotal success that does not play into the results of clinical trials – this can include the use of spectacles/contact lenses to control myopic progression and patients being on the drops for a longer period of time than the length of the study.
2. Some only use 0.01% at the start of the treatment
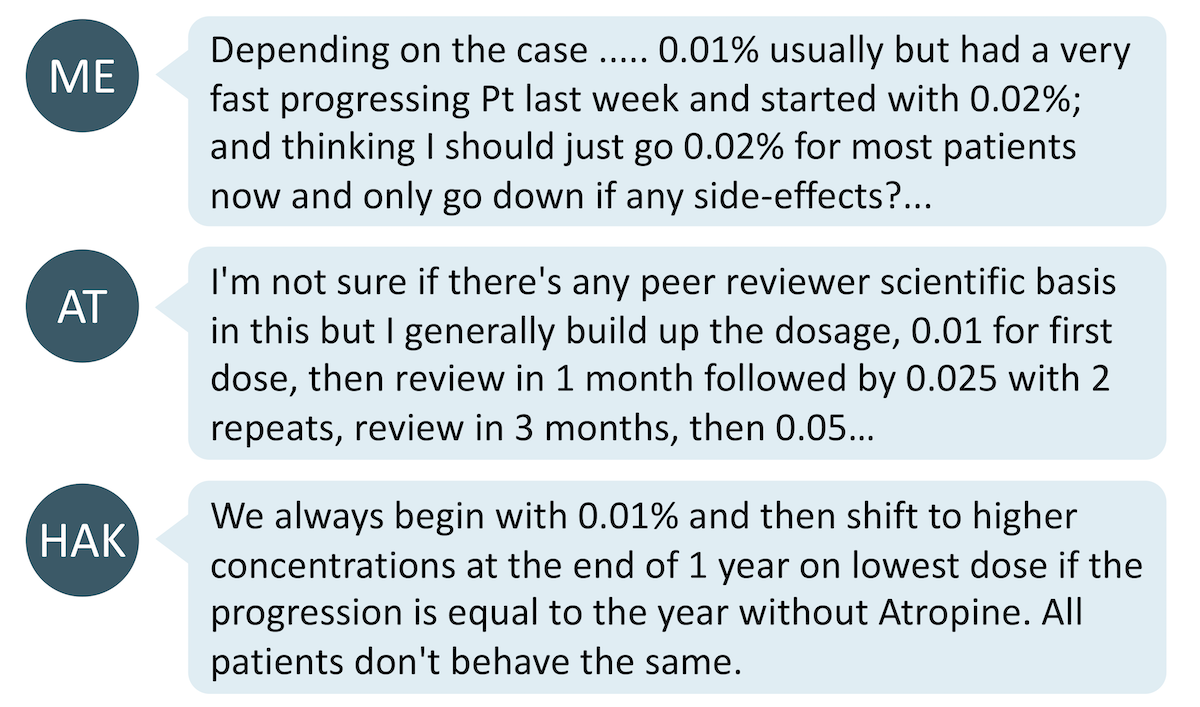
For some others, 0.01% serves as a starting point and this concentration is adjusted over time to either wean a patient onto higher concentrations, or if myopic progression is faster than desired.
3. Some believe 0.01% should not be even considered

AM's comparison with steroid treatment is interesting. It's not typical or even safe prescribing to start with a lower strength steroid and increase if the treatment isn't working, but safe prescribing also dictates the minimum strength medication should be chosen to resolve the condition. Is this a fair comparison to compare an acute event (ocular inflammation needing a steroid) versus a treatment for a non-acute condition which needs to be tolerated over the long term? This is worth reflection.
The argument against 0.01% is that recent literature suggests it does not have any effect on axial elongation, and that increased concentrations leads to greater efficacy. The aim is to prescribe minimum dosage for maximum effect on axial elongation with minimum side effects, and studies appear to show this is more likely to be around 0.025% or 0.05% with the current compounded formulations available.
The puzzling aspect of 0.01% performance in scientific studies is the mismatch between axial length and refractive control whereby there is axial length elongation whilst refractive error is unchanged. As most clinicians don’t measure axial length, they may be unwittingly administering ineffective treatment which appears successful on the face of refraction, but does not meet the goal of myopia control, which is to reduce the rate of axial length elongation.
Concern about side effects is the main barrier to prescribing higher dosages
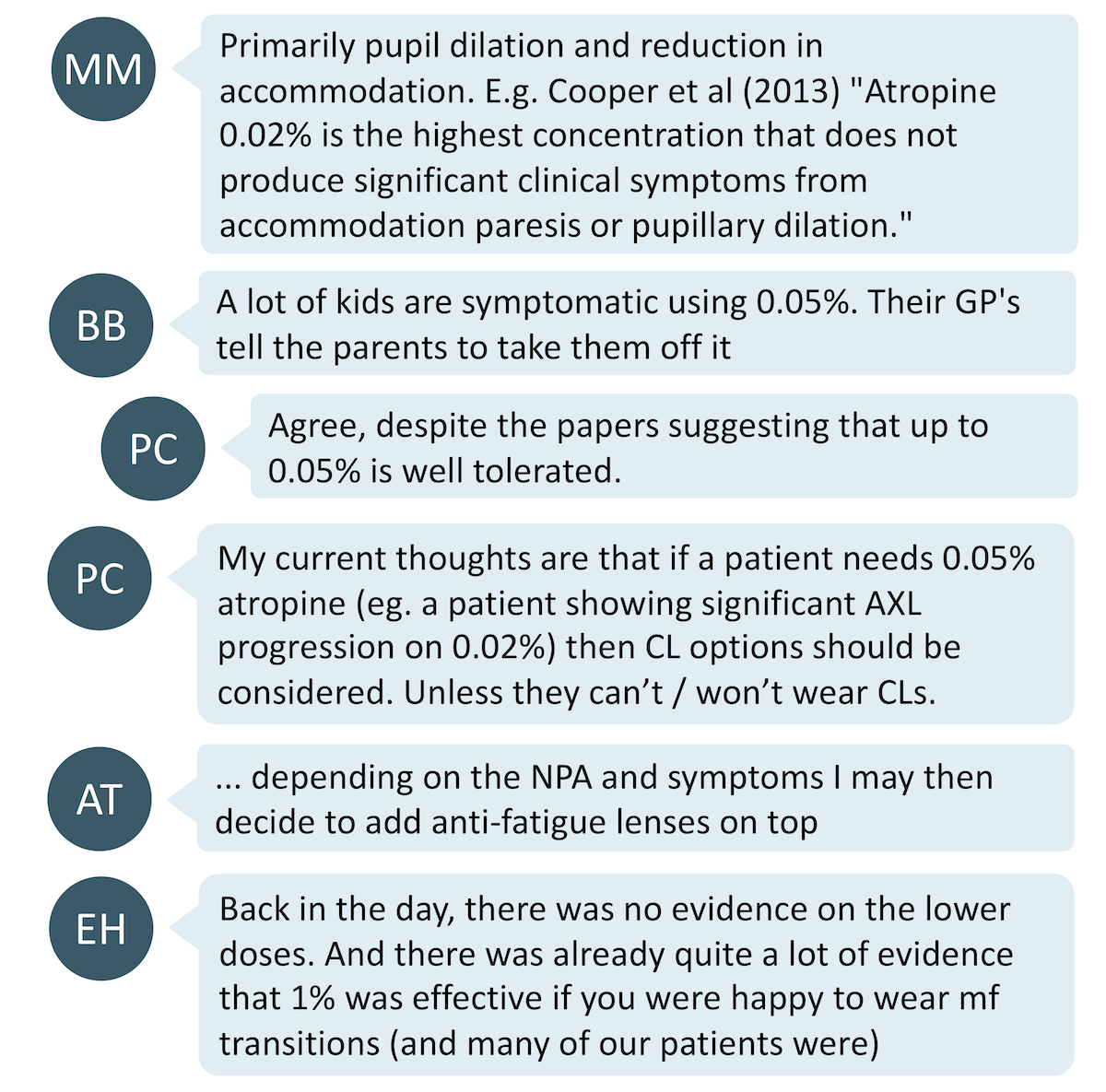
There were multiple comments that reported children having symptoms with 0.05% atropine whilst children have no issue with 0.02% or lower concentrations of atropine. Side effects of atropine most commonly include photophobia, poor near visual acuity, allergy. Other adverse effect such as headaches, chalazion and systemic effects occurred in a small minority of patients.2
Feedback from the community suggests that 0.02% atropine generally does not cause any side effects, whilst higher concentrations can bring disconcerting side effects for some patients and their parents. Some clinicians mitigate this by prescribing multifocal/bifocal spectacles to help the child with accommodation side effects, and transition lenses to reduce glare. On the other hand, PC suggested myopia control contact lens options as an adjunct if the myopia control is ineffective with 0.02% atropine instead of increasing dosage.
What does the research say?
On suggested dosage of atropine:
- LAMP Phase 21 has suggested 0.05% atropine as the maximum concentration that is well tolerated for clinical use where as ATOM23 suggested 0.01% atropine. However, there is a lack of a control group for both LAMP Phase 2 and ATOM2 studies concerning the efficacy 0.01% which casts doubt on its true efficacy.
On the side effects:
- The LAMP study1 suggests that 0.05% atropine is well tolerated. However, Cooper et al4 concluded that 0.02% atropine is the highest concentration that do not give symptoms to the children. However, it is also worth noting that the LAMP study had a far larger sample size than that done by Cooper et al. Also, blue eyed children may be more likely to suffer side effects than brown eyed children.
Take home messages:
- While the studies seem to suggest at least 0.02% atropine as being retarding the progression of axial elongation, 0.01% atropine is still the dosage of choice for some practitioners, with some reporting success with it in clinical practice. For those who choose to continue prescribing 0.01% atropine, it is important that the success of this should be measured by change of axial length instead of refractive error.
- For those who do not have access to axial length measurement devices, it is worthwhile considering starting at 0.02% atropine as a minimum dosage. This is more likely to arrest the development of axial length.
- If concerned about axial length progression occurring whilst on 0.02% atropine, yet wary about side effects of increasing dosage, consider myopia control contact lens/spectacle options as an adjunct treatment.
- Perhaps the biggest factor in this variability in performance of 0.01% is related to the stability of low concentration atropine once it's compounded. New studies are underway investigating novel formulations aiming to make atropine more stable. Until science tells us more, though, the advice above is likely to be the best evidence-based approach to atropine concentration.

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.
Read our six-part blog series on atropine
-
The latest and greatest atropine research
-
When to prescribe atropine for myopia control
-
Complications in atropine compounding
-
Complex atropine cases
-
Systemic side effects of atropine eye drops
-
Atropine - wonder or weak treatment?
Check out this additional clinical case
You can also listen to our three podcasts on atropine with world-leading researchers
-
Atropine, engaging with science and responsible practice with Professor Karla Zadnik from Ohio State University, USA.
-
More on atropine 0.01% treatment for myopia management with Professor Mark Bullimore from the University of Houston, Texas USA.
-
Atropine 0.01% for myopia management with Professor James Loughman from Technological University Dublin, and the Centre for Eye Research Ireland
This content is brought to you thanks to an unrestricted educational grant from

References:
- Yam JC, Li FF, Zhang X, Tang SM, Yip BH, Kam KW, Ko ST, Young AL, Tham CC, Chen LJ, Pang CP. Two-Year Clinical Trial of the Low-concentration Atropine for Myopia Progression (LAMP) Study: Phase 2 Report. Ophthalmology. 2019. (link)
- Gong Q, Janowski M, Luo M, et al. Efficacy and Adverse Effects of Atropine in Childhood Myopia: A Meta-analysis. JAMA Ophthalmol.2017;135(6):624–630 (link)
- Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, Tan D. Atropine for the Treatment of Childhood Myopia: Safety and Efficacy of 0.5%, 0.1%, and 0.01% Doses (Atropine for the Treatment of Myopia 2). Opthahlmology. 2012 Feb;119(2):347-54 (link)
- Cooper J, Eisenberg N, Schulman E, Wang FM. Maximum atropine dose without clinical signs or symptoms. Optometry and Vision Science. 2013 Dec 1;90(12):1467-72. (link)










