COVID-19 became a global pandemic in 2020 and spurred governments to impose home confinement in many countries. Eye care practitioners were mostly spared the full brunt of the manifestations of COVID-19 clinically, as the most common ocular sign is a mild conjunctivitis and has been reported to be self-limiting.1
However, did the mandatory home confinement imposed to control the spread of COVID-19 in fact worsen myopia? Early data from China indicates that this may be the case.2 As we know, increased outdoor activity and regular breaks plus reducing total near work time can delay the onset of myopia.3 While home confinement was imposed, opportunities for outdoor activities were limited and school education went online, leading to increased near work.2
Could these lifestyle changes have affected the efficacy of myopia management as well? MW shared a case of a patient who started myopia treatment before the home confinement and suffered significant myopic progression after 12 months.

Over the course of six months of myopia controlling contact lens wear, the child progressed by -2.00D and -1.00D in her right and left eye respectively. This is very fast progression compared to what could be expected for her age, especially considering that there is a myopia control strategy in place. The average amount of progression for a child of this age in single vision spectacles would be around -0.75D per year,4 so this much progression in six months, in a myopia control strategy, indicates a very poor result.
What are the possible reasons for progression?
1. Insufficient contact lens wear
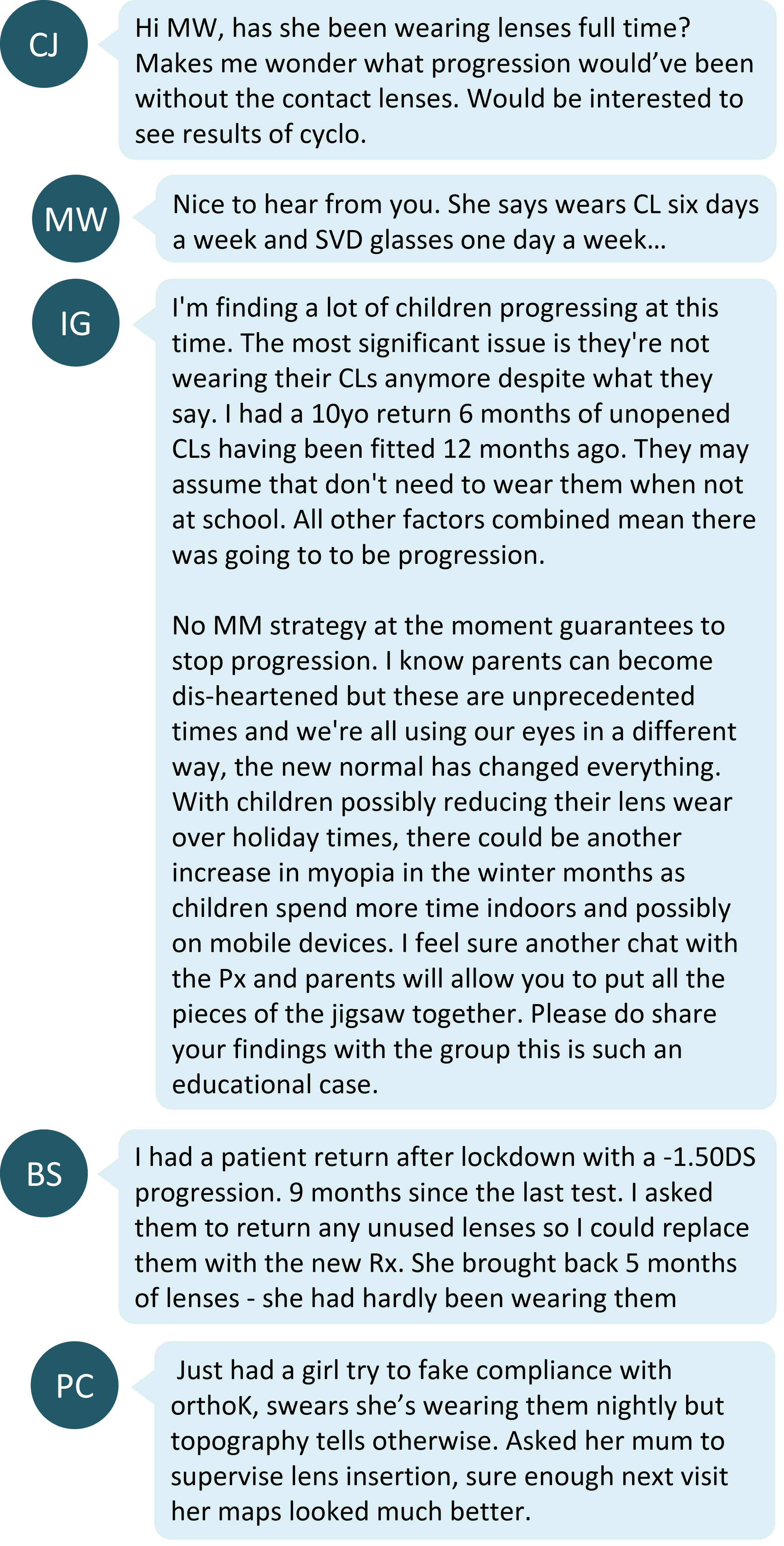
The first and most reasonable presumption is that perhaps the child has not been compliant with contact lens wear. Indeed, when schooling from home and presumably spending most of the time looking at near, the child and parent may not realize that full time wear of the myopia control strategy is still required. One study of a novel design of soft myopia controlling contact lens found a correlation between reduced wearing time and a reduced myopia controlling effect. Wearing time of at least 8 hours a day led to the best outcomes.5
The other significant effect of reduced wearing time is the child suffering undercorrection or un-correction of their myopia, which has shown a link with faster myopia progression.6
IG mentioned also that some children take a break from contact lens wear when they are on holidays. This would mean that they could be spending more time in non-myopia controlling optical correction, or in no correction, than expected. This would then explain the lack of myopia control effect. Some commenters suggested that requesting patients to bring in the balance of their contact lens supply is a good way to ascertain whether they have been compliant in keeping to advised wearing times.
2. Excess near work
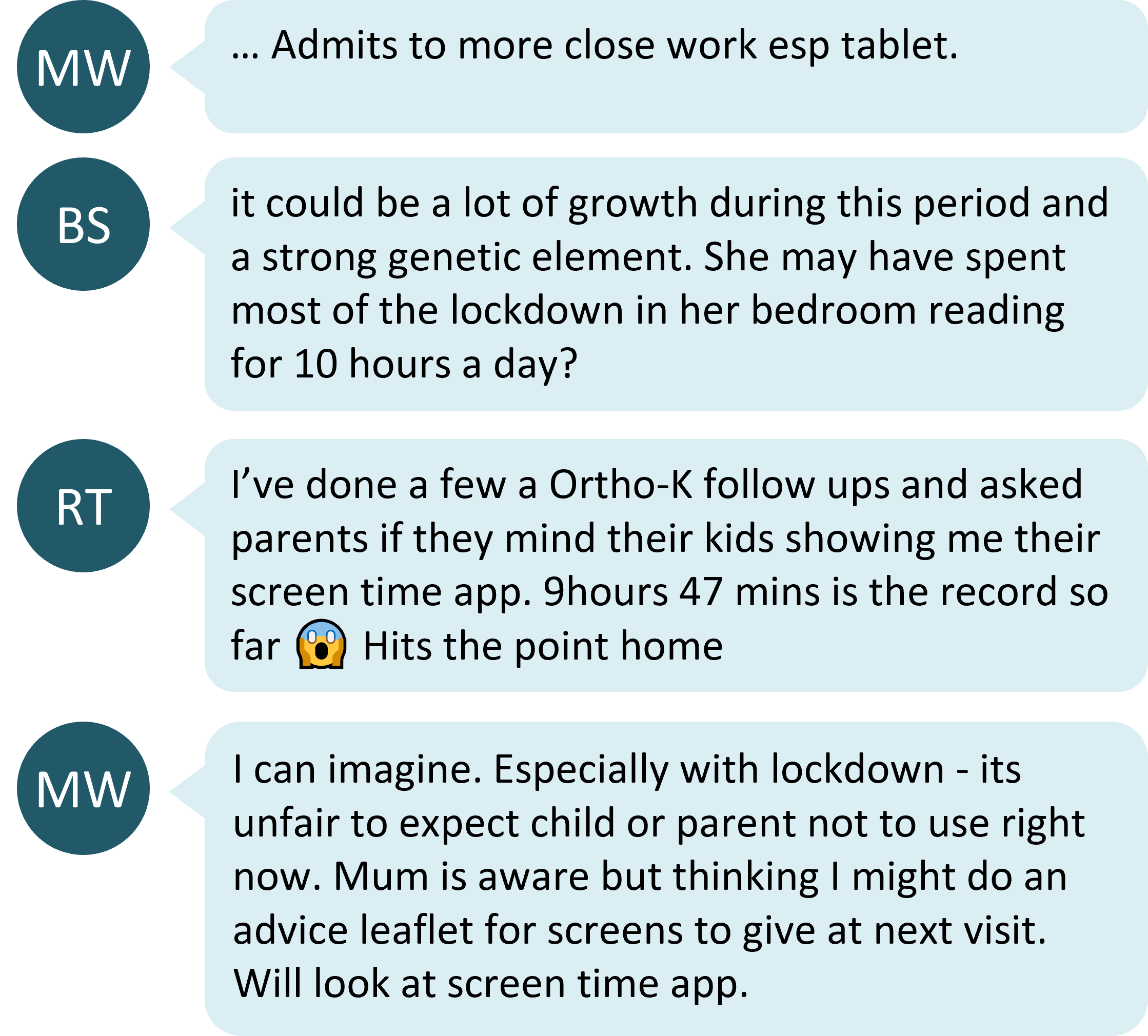
As home confinement was imposed, in-person classes were cancelled, and students were forced to learn the curriculum virtually. This led to increased screen time and near work. The impact of screen time specifically on myopia is varied according to a systemic review,6 however, there is an association between near work activities and myopia in children, where the odds of myopia are increased with the more the time spent on near activities.7
3. Genetics
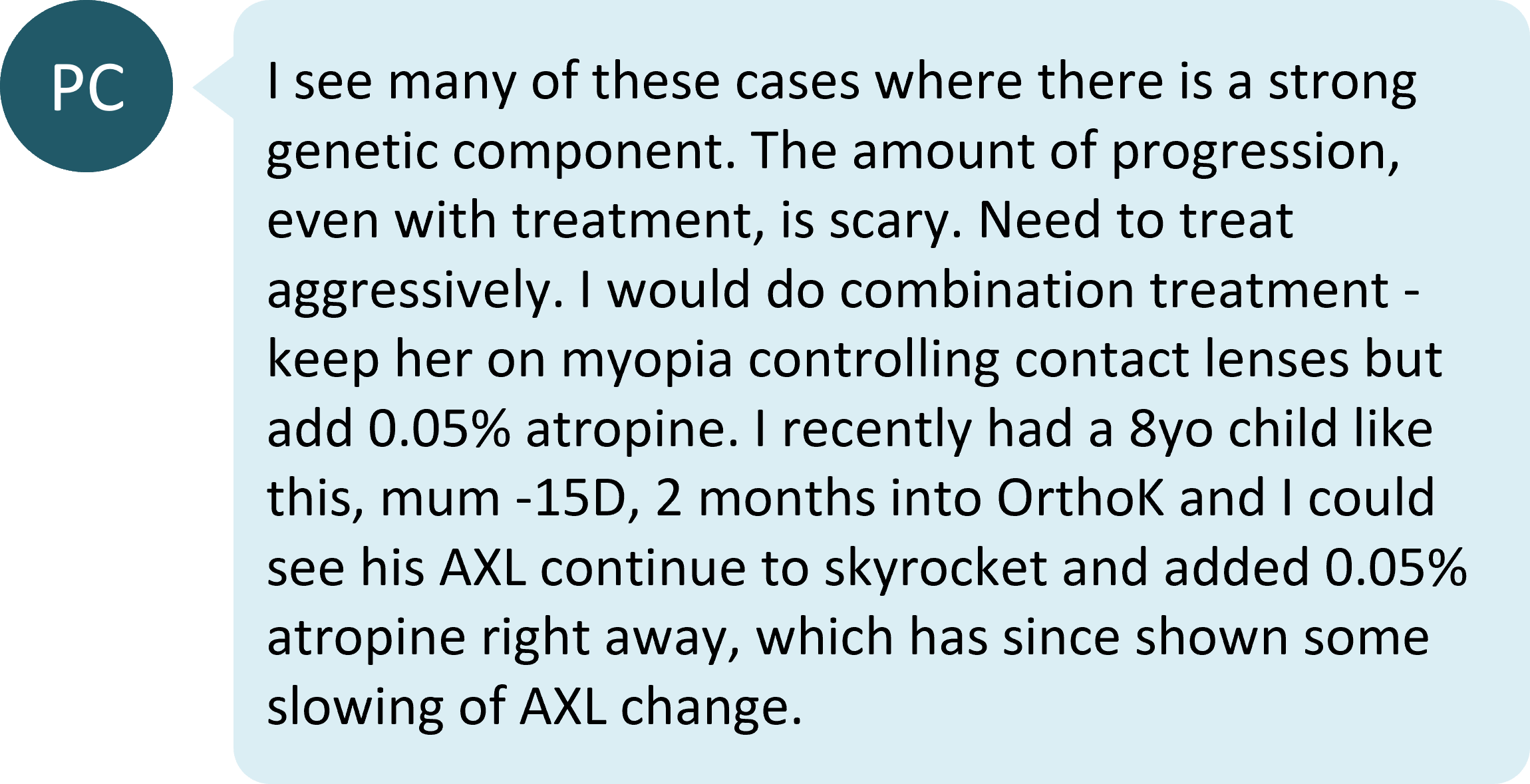
As both parents are highly myopic, this patient is at risk of faster myopia progression.9 This could lead to consideration of a more effective strategy - combination treatment with atropine is mentioned. There is growing evidence that combining atropine with orthokeratology can increase short-term myopia control efficacy, but currently no evidence base for combining atropine with other optical interventions.10
4. What else should be considered?
The original poster, MW, asks if corneal curvature measurements are important. The answer to this is yes - typically, corneal curvature doesn't change much in childhood myopia progression,11 so any contribution of steepened corneal curvature to the refractive change should be ruled out with keratometry or corneal topography. Read more about this in Are you measuring the cornea in myopia management?
Take home messages:
- There appears to be an association between home confinement and myopia progression, at least based on data from China. This may be due to reduced outdoor activity and excessive near work.
- When myopia progression is faster than expected, it is important to rule out other possible factors that influence myopia progression such as treatment compliance and the effect of visual environment. Both of these factors can be modified with the right clinical advice.
- Family history cannot be modified, but can also play a factor in faster progression. It is also important to ensure that parents understand that myopia control treatments can slow, but not stop, myopia progression in their children.
Read more about managing treatment outcomes

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.
This content is brought to you thanks to an unrestricted educational grant from
![]()
References
- Hu K, Patel J, Patel BC. Ophthalmic manifestations of coronavirus (COVID-19). StatPearls [Internet]. 2020 Apr 13. (link)
- Wang J, Li Y, Musch DC, Wei N, Qi X, Ding G, Li X, Li J, Song L, Zhang Y, Ning Y, Zeng X, Hua N, Li S, Qian X. Progression of Myopia in School-Aged Children After COVID-19 Home Confinement. JAMA Ophthalmol. 2021 Mar 1;139(3):293-300. (link)
- Tideman JW, Polling JR, Jaddoe VW, Vingerling JR, Klaver CC. Environmental risk factors can reduce axial length elongation and myopia incidence in 6-to 9-year-old children. Ophthalmology. 2019 Jan 1;126(1):127-36. (link) [Link to Myopia Profile Science Review]
- Donovan L, Sankaridurg P, Ho A, Naduvilath T, Smith EL 3rd, Holden BA. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012 Jan;89(1):27-32 (link)
- Lam CS, Tang WC, Tse DY, Tang YY, To CH. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial. Br J Ophthalmol. 2014 Jan;98(1):40-5. (link)
- Logan NS, Wolffsohn JS. Role of un-correction, under-correction and over-correction of myopia as a strategy for slowing myopic progression. Clin Exp Optom. 2020 Mar;103(2):133-137. (link)
- Lanca C, Saw SM. The association between digital screen time and myopia: A systematic review. Ophthalmic and Physiological Optics. 2020 Mar;40(2):216-29. (link)
- Huang HM, Chang DS, Wu PC. The association between near work activities and myopia in children—a systematic review and meta-analysis. PloS one. 2015 Oct 20;10(10):e0140419. (link) [Link to Myopia Profile Science Review]
- Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Familial clustering and myopia progression in Singapore school children. Ophthalmic Epidemiol. 2001 Sep;8(4):227-36. (link)
- Tan Q, Ng AL, Choy BN, Cheng GP, Woo VC, Cho P. One-year results of 0.01% atropine with orthokeratology (AOK) study: a randomised clinical trial. Ophthalmic Physiol Opt. 2020 Sep;40(5):557-566. (link)
- Mutti DO, Mitchell GL, Sinnott LT, Jones-Jordan LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K, The CLEERE Study Group. Corneal and Crystalline Lens Dimensions Before and After Myopia Onset. Optom Vis Sci. 2012;89(3):251-262. (link)











