Managing myopia typically refers to childhood myopes, but myopia management in adults presents its own challenges and considerations. Whilst the focus typically moves from slowing myopia progression to monitoring eye health in adult myopia, how do we manage refractive changes, eye health and general health factors? Here is a complex case from LM describing a young adult with aphakia and Type 1 diabetes whose myopia might be progressing.
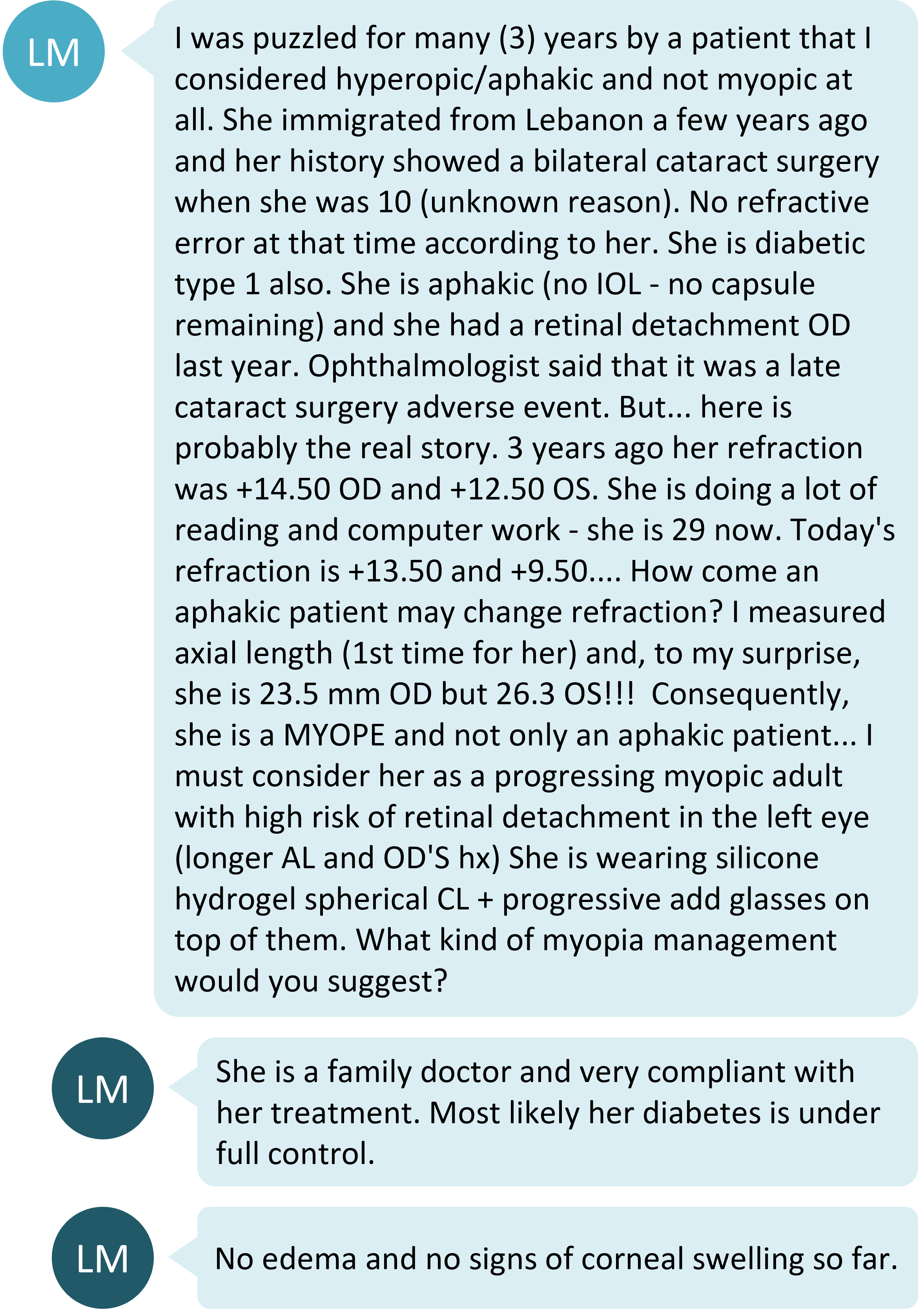
How diabetes can affect refractive error

There was much discussion about the role of diabetes in affecting this patient’s refractive error. It is common knowledge that blood glucose levels can affect refractive error - acute changes in blood glucose levels can shift refraction to either myopia or hyperopia,1 although upon intensive treatment, hyperopic shifts are more common.2 In well managed diabetes, as appears to be the case here, daily fluctuations in blood glucose levels don't appear to affect refraction.3
Refractive changes in diabetes are typically due to changes in the thickness and curvature of the crystalline lens. Corneal curvature is usually unaffected and findings on corneal thickness differences between people with diabetes and age-matched controls are equivocal.4 In this patient with aphakia, crystalline lens alteration due to diabetes is not a factor in her observed refractive changes.
If the lens is not a factor in the myopic shift observed in this patient, how can ocular measurements help to determine the cause?
Corneal curvature
The corneal curvature is not typically altered by blood glucose levels.4 For this patient, measurement of corneal curvature would help to rule out any irregularity and/or steepening which could be contributing to the refractive change. Typically keratoconus onsets in the second decade of life, but it can progress in adults.5 A case series showed 7 eyes of 4 patients with an average age of 29 years who demonstrated keratoconus progression in pregnancy.6
Axial length
This is where the clinical mystery became clearer, with axial length measurements indicating definite axial myopia in the left eye. Since an axial length of more than 26mm increases the lifetime risk of vision impairment,7 the ocular health of this 'myopic' eye must be closely monitored.
An important note is that optical biometers typically have a phakic and aphakic or pseudophakic measurement setting, as the optical path length of measurement is influenced differently by the crystalline lens compared to an intraocular or absence of lens. Measurement of an aphakic eye in the phakic mode results in an error of 0.2mm8 – if this patient had been measured in phakic mode, the true axial lengths would be 23.7mm in the right eye and 26.5mm in the left.
Is this patient a myope?
Children who undergo cataract surgery typically exhibit a myopic refractive shift which is larger when the surgery is undertaken at a younger age.9 Even though the manifest refraction is highly hyperopic, the crystalline lens normally contributes 10-15D of refractive power to the eye.10 Putting this alongside the patient's current refraction of R +13.50 and L +9.50, if the eyes were phakic, the right eye could be in the range of low myopia to moderate hyperopia. The left eye is almost certainly the equivalent of low-to-moderate myopia from a refraction point of view, and knowing that axial length is over 26mm, could be considered a high myope from a retinal point of view.7
There is little known about how axial length changes in adult myopia progression. Repeated axial length measurements, if available, would help to isolate axial growth as the cause of refractive change in this patient. Even just this single measurement, though, indicates left eye axial 'high myopia' and hence increased risk of ocular pathology,7 requiring frequent eye health monitoring. This is of utmost importance for the patient as she already has a history of retinal detachment in the right (shorter axial length) eye.
The International Myopia Institute recommends that high myopes be reviewed annually with retinal health examination through dilated pupils.11
Treatment options
Multifocal soft contact lenses

As the patient is already currently wearing soft contact lens, commenters suggested multifocal soft contact lens (MFCLs) as a form of myopia control. Others mentioned it could support her near vision. Her high hyperopic refractive error means that a customized MFCL would likely be needed, if prescribed.
MFCLs are often used to slow myopia progression in children, but there is no data on myopia control in young adults. Moreover, this patient's unusual clinical profile including aphakia and diabetes makes her fall even further outside the range of typical myopia control studies. This patient requires a full near addition due to aphakia - evidence indicates that spectacles will provide this more effectively and predictably than the 'near add' provided in MFCLs.12
Monitor refraction and eye health
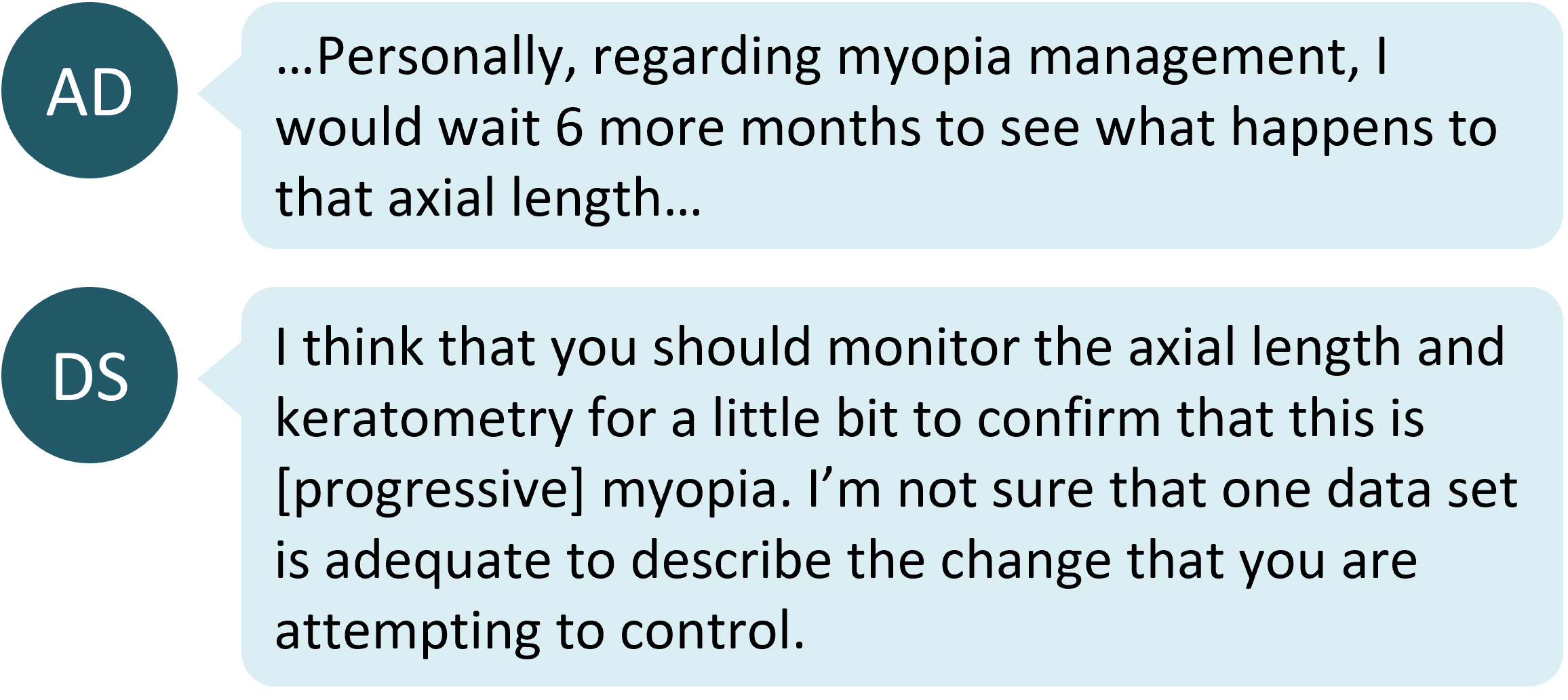
Some other commenters were less convinced that this was a case of progressing myopia and suggested repeated measurement over time, with less focus on prescribing a myopia control solution. This is sensible given the patient's unusual clinical presentation and history, but the diagnosis of left axial myopia based on the axial length measurement does require ocular health management as for a refractive myope.
The original post described that the patient's near work habits had changed. One study has shown a link between visual environment habits in childhood and adulthood, and adult myopia progression.13 The short-term impact of close reading distances on axial length has also been demonstrated.14 Hence, reinforcing the need for good visual habits such as regular breaks from near work is useful advice for this patient.
Take home messages:
- When a patient is aphakic or pseudophakic from childhood, their refractive error may not necessarily reflect the reality of their axial length - measuring this helps to gauge the related retinal health risk
- Eyes with longer axial length (over 26mm) are recommended to have an annual retinal health examination through dilated pupils to monitor ocular health, regardless of the manifest refraction.
- There is little known about the typical course and frequency of adult myopia progression and whether myopia control strategies used for children will be effective in adults. Systemic health conditions like diabetes can further add to the complexity. Consideration of the best optical correction for the patient, and then regular monitoring, may be the ideal course of management.
Further reading

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.
This content is brought to you thanks to an unrestricted educational grant from
References
- Kaštelan S, Gverović-Antunica A, Pelčić G, Gotovac M, Marković I, Kasun B. Refractive Changes Associated with Diabetes Mellitus. Semin Ophthalmol. 2018;33(7-8):838-845. (link)
- Li HY, Luo GC, Guo J, Liang Z. Effects of glycemic control on refraction in diabetic patients. Int J Ophthalmol. 2010;3(2):158-60. doi: 10.3980/j.issn.2222-3959.2010.02.15. Epub 2010 Jun 18. PMID: 22553542; PMCID: PMC3340779. (link)
- Huntjens B, Charman WN, Workman H, Hosking SL, O'Donnell C. Short-term stability in refractive status despite large fluctuations in glucose levels in diabetes mellitus type 1 and 2. PLoS One. 2012;7(12):e52947. (link)
- Huntjens B, O’Donnell C. Refractive error changes in diabetes mellitus. Optometry in Practice. 2006;7(3):103-14. (Link)
- Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS. Keratoconus: a review. Cont Lens Anterior Eye. 2010 Aug;33(4):157-66; quiz 205. (link)
- Bilgihan K, Hondur A, Sul S, Ozturk S. Pregnancy-induced progression of keratoconus. Cornea. 2011 Sep;30(9):991-4. (link)
- Tideman JW, Snabel MC, Tedja MS, van Rijn GA, Wong KT, Kuijpers RW, Vingerling JR, Hofman A, Buitendijk GH, Keunen JE, Boon CJ, Geerards AJ, Luyten GP, Verhoeven VJ, Klaver CC. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol. 2016;134(12):1355-1363. (link) [Link to Myopia Profile Science Review]
- Haigis W. Pseudophakic correction factors for optical biometry. Graefes Arch Clin Exp Ophthalmol. 2001 Aug;239(8):589-98. (link)
- Borja D, Manns F, Ho A, Ziebarth N, Rosen AM, Jain R, Amelinckx A, Arrieta E, Augusteyn RC, Parel JM. Optical power of the isolated human crystalline lens. Invest Ophthalmol Vis Sci. 2008 Jun;49(6):2541-8. (link)
- Crouch ER, Crouch Jr ER, Pressman SH. Prospective analysis of pediatric pseudophakia: myopic shift and postoperative outcomes. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2002 Oct 1;6(5):277-82. (link)
- Gifford KL, Richdale K, Kang P, Aller TA, Lam CS, Liu YM, Michaud L, Mulder J, Orr JB, Rose KA, Saunders KJ, Seidel D, Tideman JWL, Sankaridurg P. IMI - Clinical Management Guidelines Report. Invest Ophthalmol Vis Sci. 2019 Feb 28;60(3):M184-M203. (link)
- Kim E, Bakaraju R, Ehrmann K. Power Profiles of Commercial Multifocal Soft Contact Lenses, Optometry & Vision Science. 2017 Feb 94(2):183-96. (link)
- Pärssinen O, Kauppinen M, Viljanen A. The progression of myopia from its onset at age 8-12 to adulthood and the influence of heredity and external factors on myopic progression. A 23-year follow-up study. Acta Ophthalmol. 2014 Dec;92(8):730-9. (link)
- Woodman EC, Read SA, Collins MJ, Hegarty KJ, Priddle SB, Smith JM, Perro JV. Axial elongation following prolonged near work in myopes and emmetropes. British Journal of Ophthalmology. 2011 May 1;95(5):652-656. (Link)











