SN shared a clinical case on our Facebook group that involved managing extreme anisometropia. This involved a 9-year-old anisometropic amblyope with dry eyes. Given the complex presentation, this was an interesting case for the Myopia Profile community to discuss.
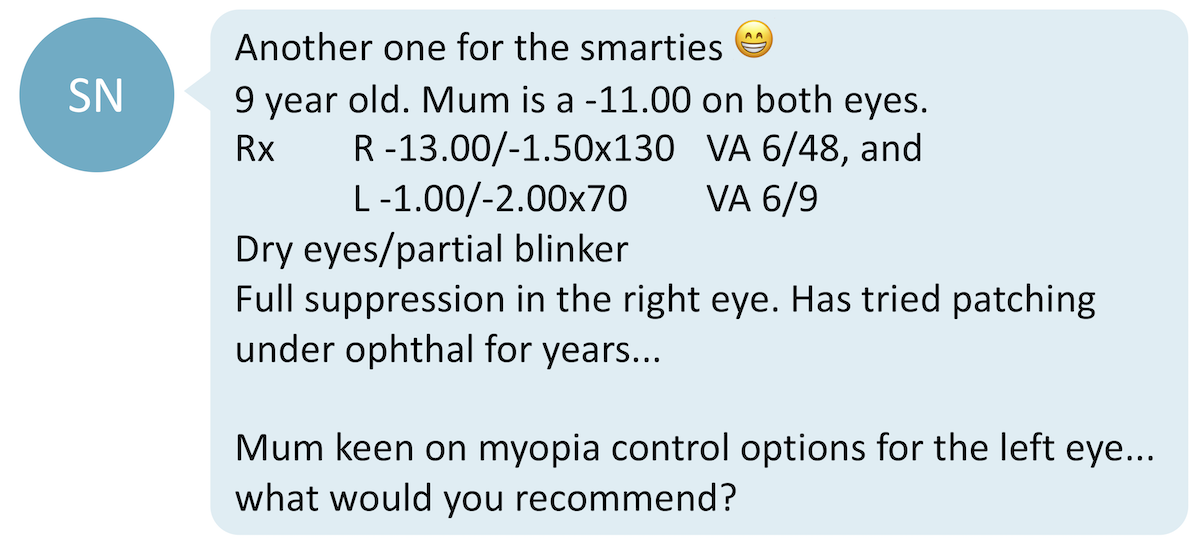
This case is not your typical astigmatic myope. There are several features to this patient that require careful consideration.
Step 1: Investigate the pathology behind the high myopia and amblyopia before deciding on myopia management
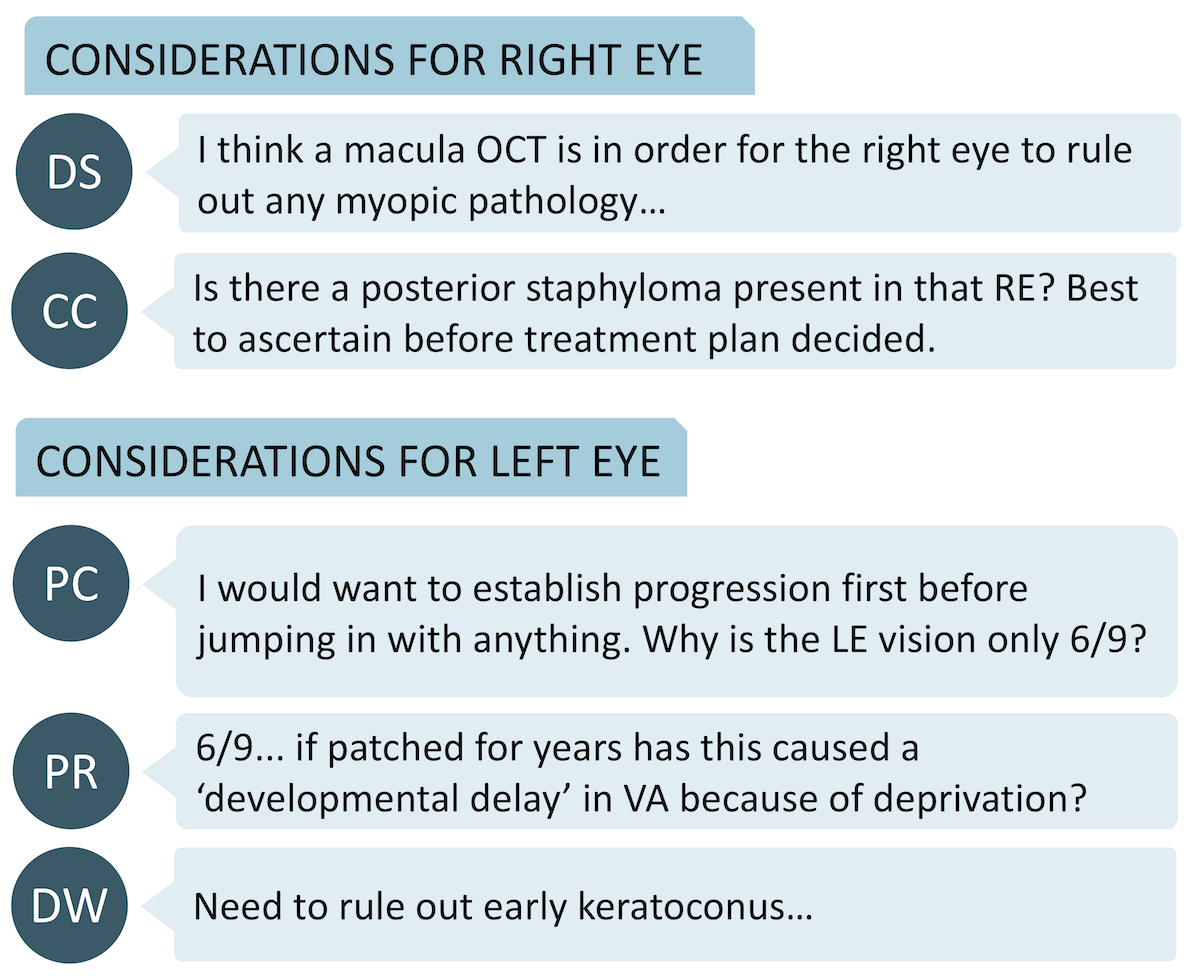
As the patient has high myopia on the right eye, extra tests need to be carried out as unilateral high myopia is often associated with abnormality of the eye1. On the other hand, the slightly reduced VA on left eye warrants investigation.
Extra tests to consider are:
- OCT (macula): to rule out myopic pathology in RE and other causes for reduced VA in LE
- A-scan: axial length difference between eyes
- B-scan: to rule out posterior staphyloma in RE
- Topography: to investigate whether irregular astigmatism is contributing to reduced VA in LE
Step 2: Myopia correction and management
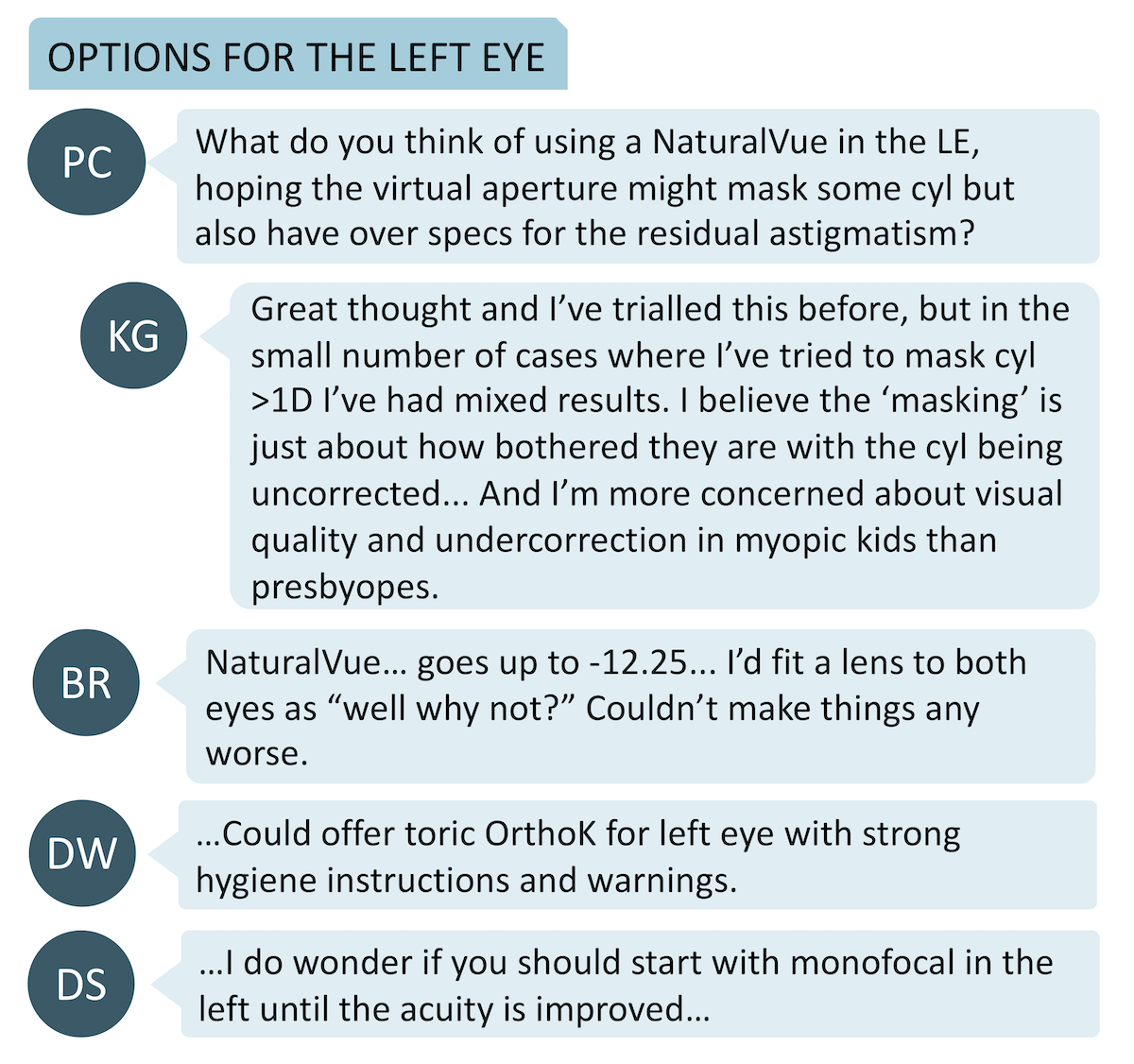
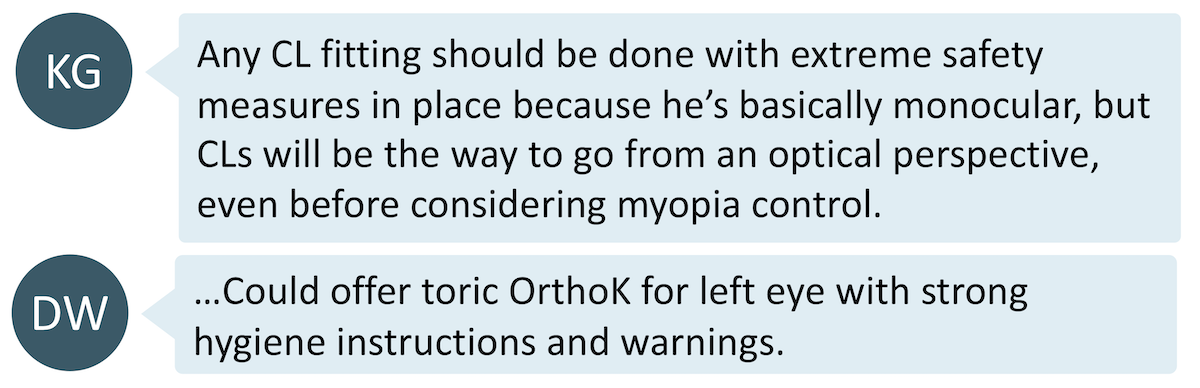
Due to the large degree of anisometropia, contact lens treatment was considered the first option for vision correction as it would eliminate image size issues that come with glasses. The very high RE myopia is also likely to benefit from contact lens wear to achieve better acuity than spectacle lens wear, presuming no other cause to the amblyopia such as strabismus or pathology. The community proposed both soft contact lens and OrthoK to SN. The thought process for each eye is different, so let’s look at them individually.
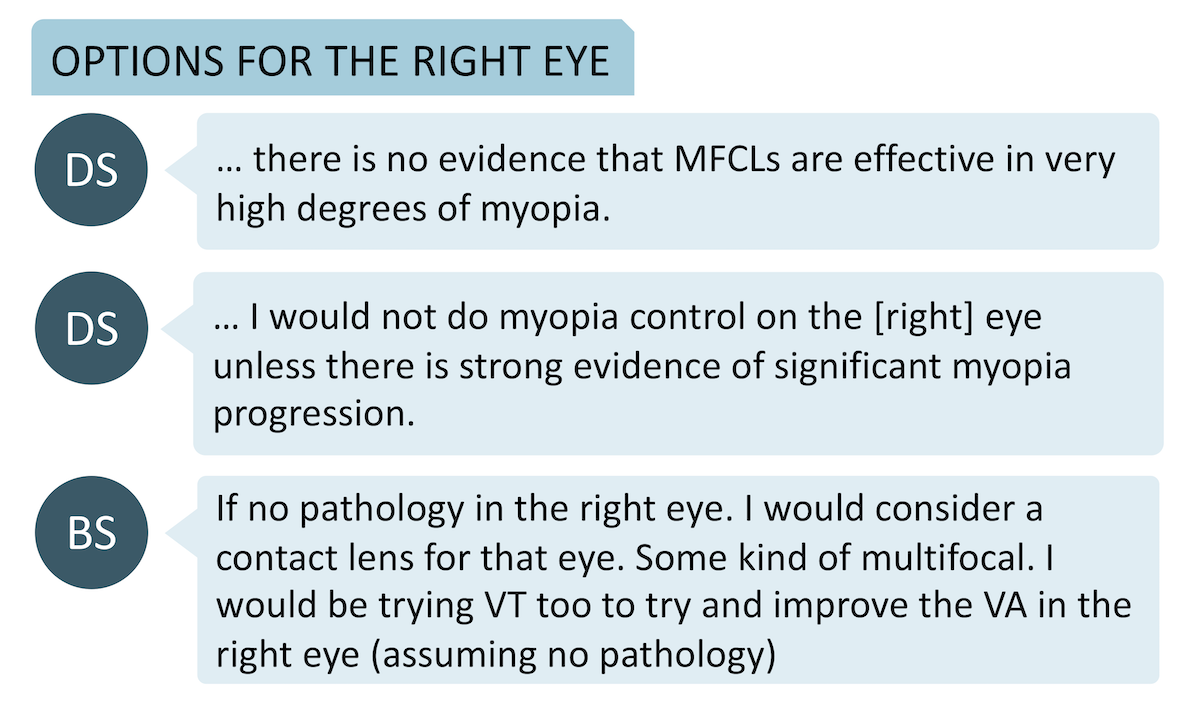
This is the amblyopic eye with very high myopia. Considerations before deciding on management for this eye include:
- Is there any pathology?
- Is the myopia in this eye still progressing?
- Is it worthwhile initiating myopia control strategies on an eye that is amblyopic?
There was significant discussion as to whether it is worthwhile fitting a MFCL to this eye. Doing so may potentially retard further myopic progression even though current literature for myopia control efficacy does not cover this power range. However, the optics of a MFCL could influence any possible improvement in VA in that eye - achieving optimum acuity may be the first priority.
Options for myopia control include:
Soft contact lens
- A toric soft MFCL was suggested but may be difficult to fit. There are also no daily disposable options for this.
- Spherical MFCLs may able to mask some astigmatism, particularly the NaturalVue due to its specific small central optic, depth of focus design. However, the anecdotally reported results vary between individuals.
OrthoK
- Whether to undertake spherical OrthoK or toric OrthoK depends on the result of topography. Research by Zhang et al2 suggests toric periphery OrthoK designs give similar visual acuity, better treatment zone centration and lower incidence of corneal staining in myopic children with moderate-to-high corneal astigmatism.
- Before commencing this, make sure keratoconus is ruled out.
- This may better correct the astigmatism compared to soft contact lens options, depending on corneal shape.
Step 3: Considering and Communicating Safety and Risk
Amblyopia effectively leaves this patient with only one good ‘seeing’ eye. Dry eyes and partial blinking could elevate the risks associated with contact lens wear, hence the safety and risk profile must be communicated clearly with the patient and parent before commencing treatment. The risk of microbial keratitis between the various CL options differ - similar for OrthoK and reusable MFCLs, and less for daily disposables - it is important to assess the potential benefit against the risk of the CL option chosen. More references to help you with this are below.
What the research says:
- Currently, there is no research available that investigates the efficacy myopia control strategies in extremely high myopia. Most myopia control clinical trials do not study myopia worse than -7.00D3.
- There are also no studies available that investigate myopia control strategies in the context of myopia in an amblyopic eye.
- The incidence rate of microbial keratitis (MK) in daily disposables CL wearers is 1 per 5,000 patient wearing years.4 The risk of MK in reusable, silicon hydrogel daily wear contact lenses is around 1 per 1,000 patient wearing years,4 and this is similar to the risk of paediatric OrthoK wear.5 See the 'References to help' section below for more.
Take home messages:
- Check for ocular pathology in unilateral high myopia
- There is currently no evidence on the efficacy of myopia control strategies in power ranges exceeding -7.00D. While some effort to control myopia is better than none, it is important to communicate this effectively to parents and properly weigh up the risk, cost and benefit to initiating myopia control in this power range. You may instead wish to simply focus on achieving the best corrected visual acuity in a highly myopic, amblyopic eye
- Ensure acuity makes sense. The slightly reduced acuity in the left eye mustn't be overlooked as this could influence safety of various contact lens choices
- The stakes are higher with an amblyopic patient! The importance of hygiene and safe contact lens wear must be communicated clearly to the patient and guardian.
References to help:
Read more on contact lens safety in children here, and check out our Myopia Management Guidelines Infographic for help on clinical communication of contact lens risks and safety.

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.
This content is brought to you thanks to an unrestricted educational grant from
References
- Weiss AH. Unilateral high myopia: optical components, associated factors, and visual outcomes. British Journal of Ophthalmology 2003;87:1025-1031. (link)
- Zhang Y, Chen YG. Comparison of myopia control between toric and spherical periphery design orthokeratology in myopic children with moderate-to-high corneal astigmatism. International Journal of Ophthalmology 2018;11(4):650–655. (link)
- Wolffsohn JS, Kollbaum PS, Berntsen DA, Atchison DA, Benavente A, Bradley A, Buckhurst H, Collins M, Fujikado T, Hiraoka T, Hirota M. IMI–Clinical myopia control trials and instrumentation report. Investigative ophthalmology & visual science. 2019;60(3):M132-60. (link)
- Stapleton F, Keay L, Edwards K, Naduvilath T, Dart JK, Brian G, Holden BA. The incidence of contact lens–related microbial keratitis in Australia. Ophthalmology. 2008 ;115(10):1655-62. (link)
- Bullimore MA, Sinnott LT, Jones-Jordan LA. The risk of microbial keratitis with overnight corneal reshaping lenses. Optometry and Vision Science. 2013;90(9):937-44. (link)











