Here is a case regarding a child with high myopia, which was presented by NK to the Myopia Profile Facebook Community. What should you do to best manage a patient like this? The findings and recommendations of the International Myopia Institute (IMI) are applied to this complex case, with links provided to the Clinical Summaries of these papers, each of which is available to download in multiple languages. Here are the clinical details of this case.
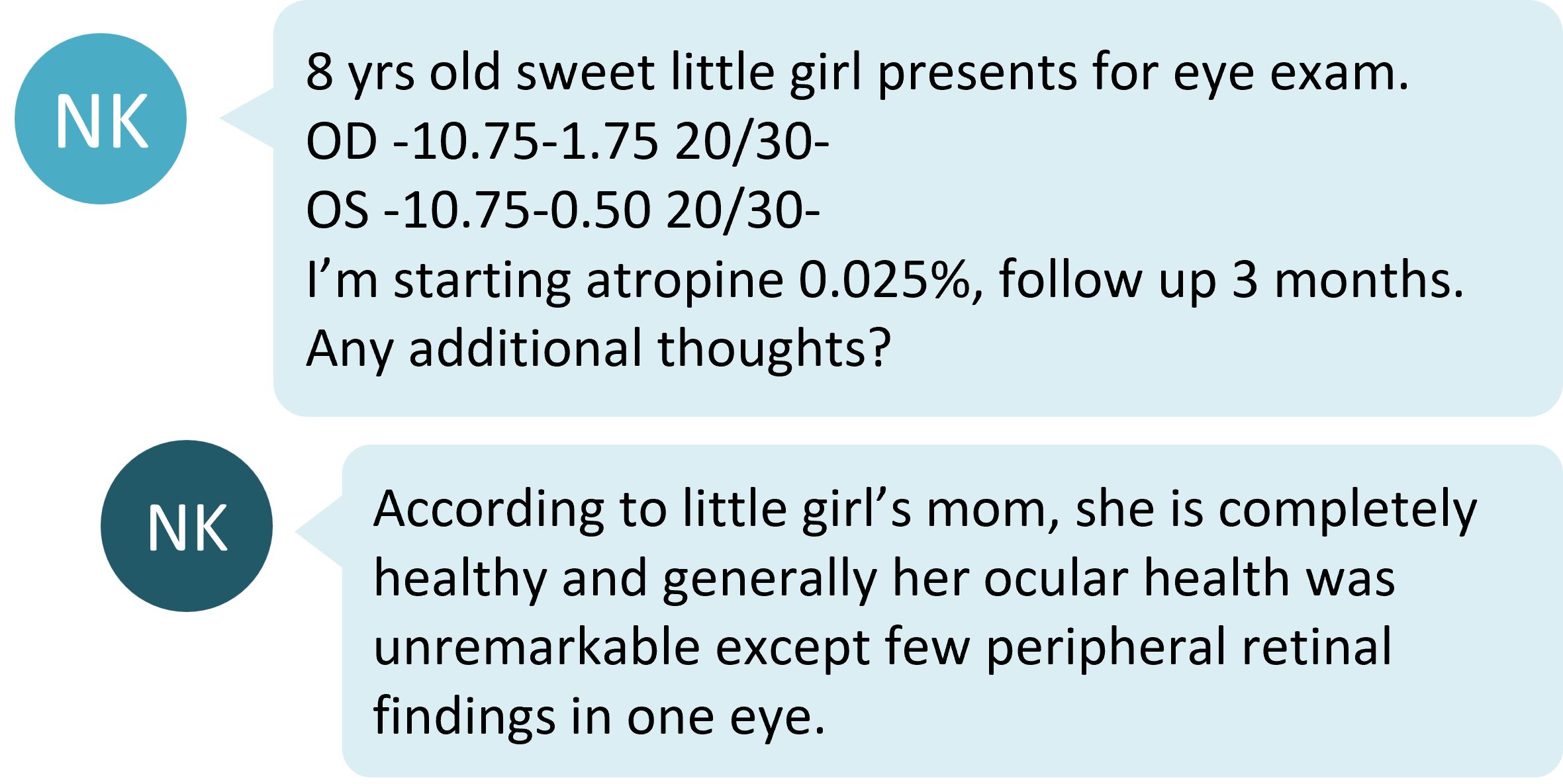
Discuss ocular health and consider systemic conditions
Syndromic myopia is defined as when myopia is associated with at least one other systemic condition.1 A referral to a paediatric ophthalmologist is warranted to investigate for possible systemic disease in cases of high myopia in children, especially children under 10 years of age.
A key educational message for patients with high myopia (and their parents or carers) is the risk of ocular disease and pathologic myopia. Whilst often misconstrued as synonymous with high myopia, pathologic myopia is defined by the International Myopia Institute (IMI), is 'an excessive axial elongation associated with myopia that leads to structural changes in the posterior segment of the eye'. These changes include myopic maculopathy, posterior staphyloma, high-myopia-associated optic neuropathy and retinal degenerations, and can occur even in eyes with lower levels of refractive myopia.2
The IMI Pathologic Myopia Report states that "83% of adults with pathologic myopia and myopic maculopathy had already had diffuse choroidal atrophy around the optic disc in their childhood. This finding suggested the possibility that children who eventually develop pathologic myopia may be different, even at an early age."2
Around half of patients with high myopia will go on to develop pathologic myopia.2 In practice, this means that even young patients with high myopia should have their ocular health closely monitored. The IMI Clinical Management Guidelines Report recommends annual retinal health examination, through dilated pupils, for patients with high myopia.3
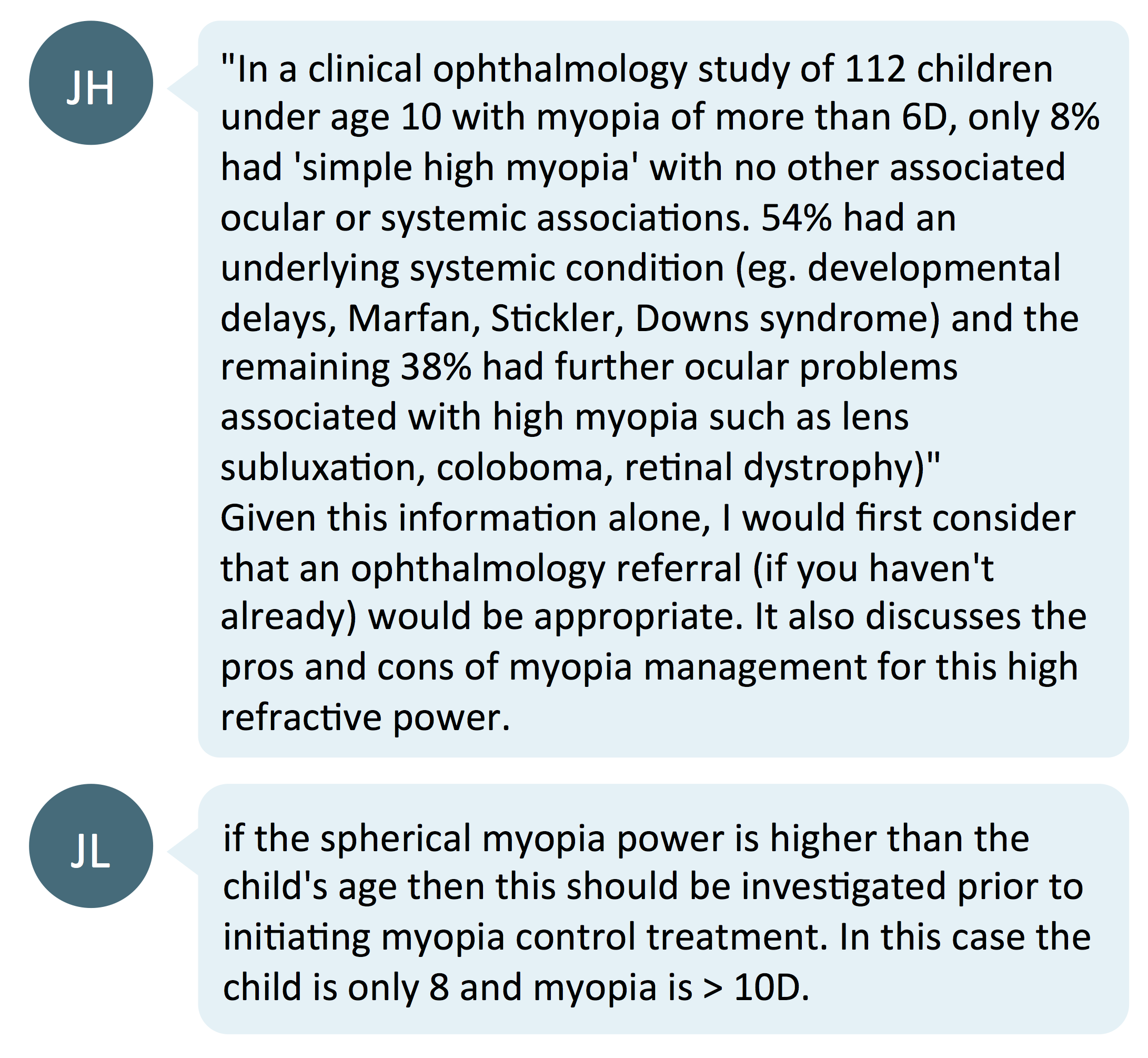
Does atropine work for high myopes?
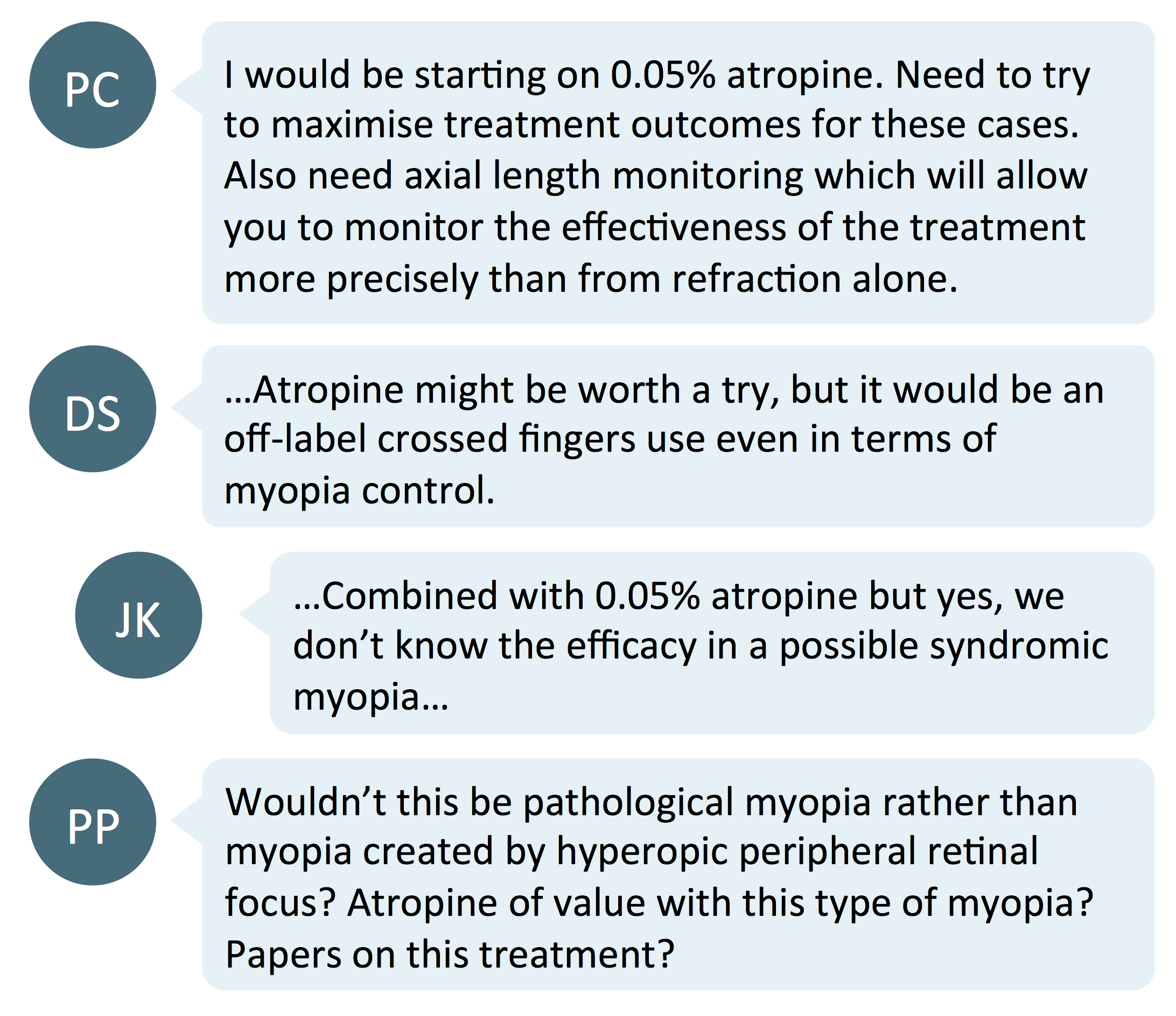
Commenters suggested to change the atropine dosage to 0.05%, instead of 0.025% as originally suggested, to increase the efficacy of myopia control. The LAMP Study showed that 0.05% atropine is most effective concentration for slowing myopia and axial elongation with minimal side effects, when compared with lower concentrations.4
However, the commenters also raised the caveat pertaining to the effectiveness of low-dose atropine in very high myopia. Most myopia control studies exclude very high myopes, like this patient. Stronger concentrations of 0.5% have been employed in a clinical protocol set forward by a Netherlands research group, with the focus on treating children at risk of high myopia based on their axial length percentiles. No comment was made of treatment for children who already present with high myopia.5
The LAMP Study specified no higher limit to myopia in their inclusion criteria, but the mean level of myopia at commencement of the study was just under -4.00D, and no correlations between level of myopia and myopia control efficacy.4
All of this means that parents must be made aware of the lack of evidence for atropine's effectiveness in very high myopia, if this treatment is to be selected.
Optical correction for high myopes
When refracting and prescribing spectacles for high myopes, it's important to control the vertex distance to achieve the best possible visual outcome. High index lenses will improve visual quality and comfort for high myopes. More tips on refraction and dispensing can be found in this Points de Vue article entitled High Myopia: the specificities of refraction and optical equipment.
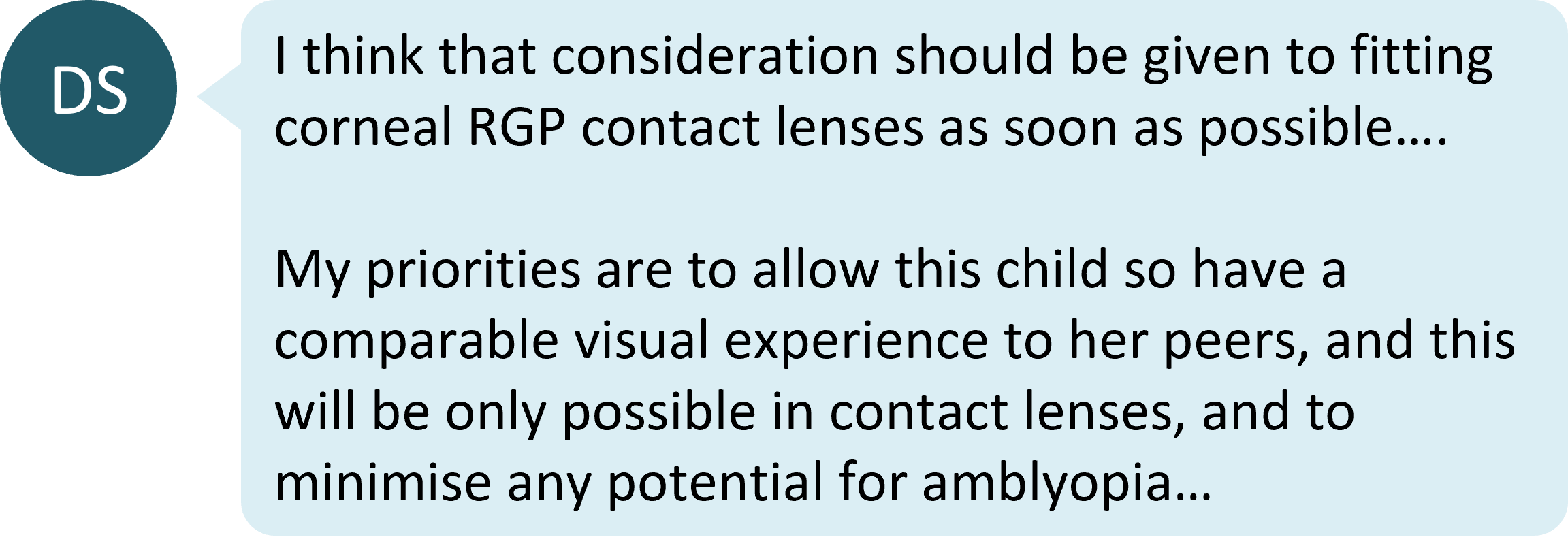
Contact lenses can improve distance acuity and field of view in high myopia, and hence are an important correction option. For both spectacles and contact lenses, there are options available which can both correct the myopic refractive error and control myopia progression. More details are provided in the IMI Prevention of Myopia and its Progression Report.6
As mentioned above with respect to atropine, it is rare that a child with such high myopia is included in myopia control studies of spectacle or contact lens treatments. Without a strong evidence-base, it could be prudent to prioritize the child achieving their best possible visual acuity ahead of a myopia control treatment, as suggested by the commenter above. The final decision on this will depend on the individual child, what treatments the eye care practitioner has available to them, and other clinical and patient-specific factors. Read more on this topic in How Should We Manage High Myopia?
Take home messages:
- A key message for patients with high myopia is the need for ongoing monitoring of ocular health. In children, this includes working with paediatric ophthalmologists to rule out any systemic associations of childhood high myopia.
- Typical myopia control strategies may or may not work for high myopes - there are few instances where children with high myopia have been included in these studies. Parents need to be aware that the 'average' expected results may not apply for their highly myopic children.
- It is important to ensure high myopes can achieve the clearest vision possible. This can be achieved through careful control of the vertex distance during refraction and spectacle dispensing; prescribing high index spectacle lenses; and considering contact lens fitting.

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.
This content is brought to you thanks to an unrestricted educational grant from
![]()
References:
- Flitcroft DI, Loughman J, Wildsoet CF, Williams C, Guggenheim JA; CREAM Consortium. Novel Myopia Genes and Pathways Identified From Syndromic Forms of Myopia. Invest Ophthalmol Vis Sci. 2018;59(1):338-348. (link)
- Ohno-Matsui K, Wu PC, Yamashiro K, Vutipongsatorn K, Fang Y, Cheung CMG, Lai TYY, Ikuno Y, Cohen SY, Gaudric A, Jonas JB. IMI Pathologic Myopia. Invest Ophthalmol Vis Sci. 2021 Apr 28;62(5):5. Erratum in: Invest Ophthalmol Vis Sci. 2021 Jun 1;62(7):17. (link)
- Gifford KL, Richdale K, Kang P, Aller TA, Lam CS, Liu YM, Michaud L, Mulder J, Orr JB, Rose KA, Saunders KJ, Seidel D, Tideman JWL, Sankaridurg P. IMI - Clinical Management Guidelines Report. Invest Ophthalmol Vis Sci. 2019 Feb 28;60(3):M184-M203. (link)
- Yam JC, Jiang Y, Tang SM, Law AK, Chan JJ, Wong E, Ko ST, Young AL, Tham CC, Chen LJ, Pang CP. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019 Jan 1;126(1):113-24. (link)
- Klaver C, Polling JR; Erasmus Myopia Research Group. Myopia management in the Netherlands. Ophthalmic Physiol Opt. 2020 Mar;40(2):230-240. (link)
- Jonas JB, Ang M, Cho P, Guggenheim JA, He MG, Jong M, Logan NS, Liu M, Morgan I, Ohno-Matsui K, Pärssinen O, Resnikoff S, Sankaridurg P, Saw SM, Smith EL 3rd, Tan DTH, Walline JJ, Wildsoet CF, Wu PC, Zhu X, Wolffsohn JS. IMI Prevention of Myopia and Its Progression. Invest Ophthalmol Vis Sci. 2021 Apr 28;62(5):6. (link)











