We know that increased levels of myopia are associated with increased risk of myopic pathologies, like retinal detachment and myopic maculopathy.1 We also know that the association is more with axial length than with dioptres,2 as two -4D myopes could have different axial lengths depending on the powers of the individual’s cornea and crystalline lens. But since most of us aren’t measuring axial length in practice, we use myopic dioptres as a surrogate. They’re a pretty good surrogate, as generally more D means more mm and myopia progression is easily measured in D.
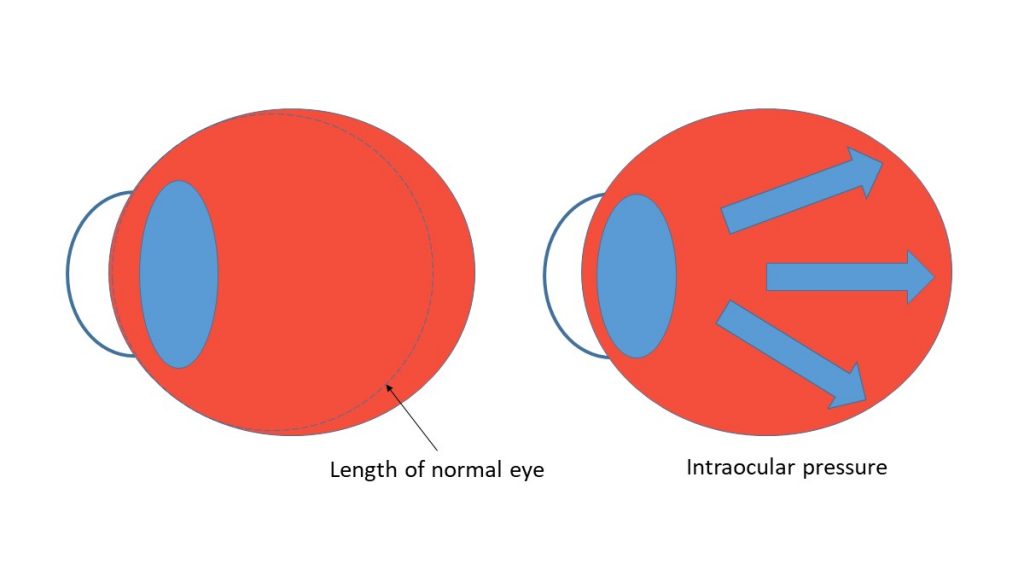
So higher dioptres means more risk of pathology and vision impairment, but it’s not guaranteed for an individual, although the relationship is clear across a population.1 Similarly, higher IOP means more risk of vision impairment from glaucoma, but as we know there’s normal tension glaucoma, and ocular hypertension which may not advance to glaucoma. Just as our -4D myope might have an axial length greater than 26mm, the next -4D could have an axial length less than 26mm if his or her myopia is more refractive (cornea and lens power) than axial. In the same way, two patients with an IOP of 26mmHg may have a different profile of risk for glaucoma, especially if one of them has a thicker cornea, reducing our index of concern.
Explaining it
Explaining the future risks of progressing myopia may seem like a large undertaking on the face of it. Firstly you have to explain that a child has myopia, what that means and how to correct it. Then you have to explain that myopia is likely to progress, and the eye health imperative of why this needs to be managed. Then you may have to introduce contact lens or pharmacological options to parents or patients who came into your consultation room not long ago, simply expecting a pair of glasses.
I’m sure it’s safe to say that we’re all good at explaining glaucoma, and its lifelong eye health risks, even though IOP isn’t a clear cut diagnostic factor. In the same way, we can be just as good as explaining that more myopic dioptres, like IOP, increase eye health risk. Despite the fact that there’s no guarantee that your -4 patient will suffer maculopathy or retinal detachment in their lifetime, the risks are real, as they are for our patient with an IOP of 26mmHg, depending on their individual presentation.
What's 'normal' axial growth?
Recently, optometrist Joe Tanner (Coopervision Aust/NZ Professional Services Manager) and I lectured on myopia management, the Misight lens and putting multifocal soft contact lenses into practice around Australia. There was an excellent question from a colleague at the Brisbane lecture on how much axial elongation is normal per year, due of the emmetropization process. The answer is we’re not 100% sure, but analysis of the enormous CLEERE study data set, presented by Don Mutti at the International Myopia Conference in 2017, indicated that around 0.1mm per year is normal for emmetropizing kids (up to age 12, give or take).3 This means that you get 0.1mm growth per year ‘for free’ before any elongation more than that could indicate myopia progression. For younger kids this axial growth ‘for free’ is a bit more than 0.1mm/year, as their eyes grow faster, and for older kids it’s a bit less. The Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study tracked thousands of kids in the USA over 10 years, examining loads of factors in refractive development, and has generated an important volume of papers over the past decade or so. One of the key distinctions in the CLEERE study has been separating the groups into children who stayed emmetropic, or became myopic. This has revealed important factors in the normal emmetropization process versus the process that leads towards myopia development – one key factor being that a child exhibiting +0.75 or less hyperopia at age 6-7 is at greatest risk of future myopia, independent of family history, ethnicity and other optical and environmental factors.4
In the multicentre 3 year Coopervision Misight study, Joe explained that the group wearing Misight lenses showed axial elongation equivalent to the group who stayed emmetropic in the CLEERE study.5 As a group, their myopia did progress by around -0.50D over three years, and their axial length increased, but similarly to an age matched group of emmetropes. By comparison, the kids wearing the single vision Proclear (control) lens showed equivalent progression to their CLEERE study counterparts who were became or were myopic, progressing by a group average of around -1.25D over three years.
We are still learning what ‘normal’ looks like for childhood axial elongation, and eventually this could be factored into myopia control studies – or in fact, factored out, as the ‘normal’ axial elongation could be removed from measures of axial progression in both treatment and control groups. If all of this is making you dubious of myopia control in general, this is not the intention – IOP isn’t a perfect measure either, but it’s the one measurement we have in our power to control, when managing glaucoma. Once there’s a more affordable instrument for us to measure axial length (nudge nudge, wink wink industry friends!!) then we’ll be able to better answer the question of how much axial length change is normal per year in children. I expect, though, that this might be a bit like IOP as well - high is bad, low is good and there is a lot of individual variation in the middle.

About Kate
Dr Kate Gifford is a clinical optometrist, researcher, peer educator and professional leader from Brisbane, Australia, and a co-founder of Myopia Profile.
References
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31:622-60. (link)
- Tideman JW, Snabel MC, Tedja MS, van Rijn GA, Wong KT, Kuijpers RW, Vingerling JR, Hofman A, Buitendijk GH, Keunen JE, Boon CJ, Geerards AJ, Luyten GP, Verhoeven VJ, Klaver CC. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol. 2016;134(12):1355-63. (link)
- Mutti DO. Endpoints in myopia control studies Ophthal Physiol Opt. 2017:Conference proceedings IMC. (link)
- Jones-Jordan LA, Sinnott LT, Manny RE, Cotter SA, Kleinstein RN, Mutti DO, Twelker JD, Zadnik K, Ethnicity tCLEo, Refractive Error Study Group. Early Childhood Refractive Error and Parental History of Myopia as Predictors of Myopia. Invest Ophthalmol Vis Sci. 2010;51(1):115-21. (link)
- Chamberlain P. Misight 3-year Clinical results. Presented at BCLA 2017, Liverpool, UK. 2017. (link)