Do pseudophakic children need myopia control options when their myopia progresses? Removing congenital cataract does not stop the growth of axial length and corneal flattening which is typical in childhood. However, the crystalline lens thinning in phakic children, which balances with axial elongation in the emmetropization process, does not happen in pseudophakes. So is an increase in myopia considered true myopia progression?
It’s an interesting conundrum that LB presented for discussion in the Myopia Profile Facebook community. Here are the details:
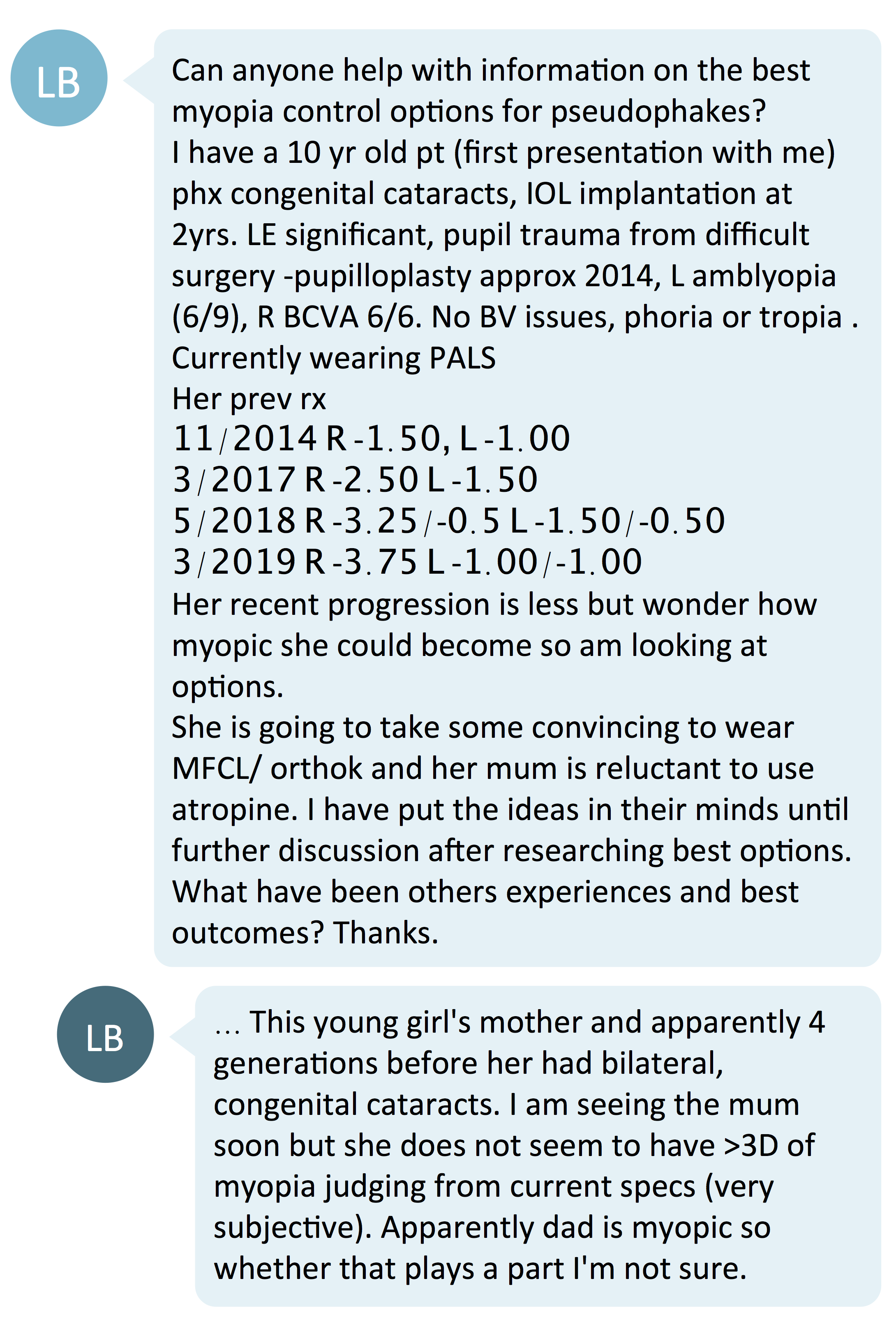
Myopic shift or emmetropization?
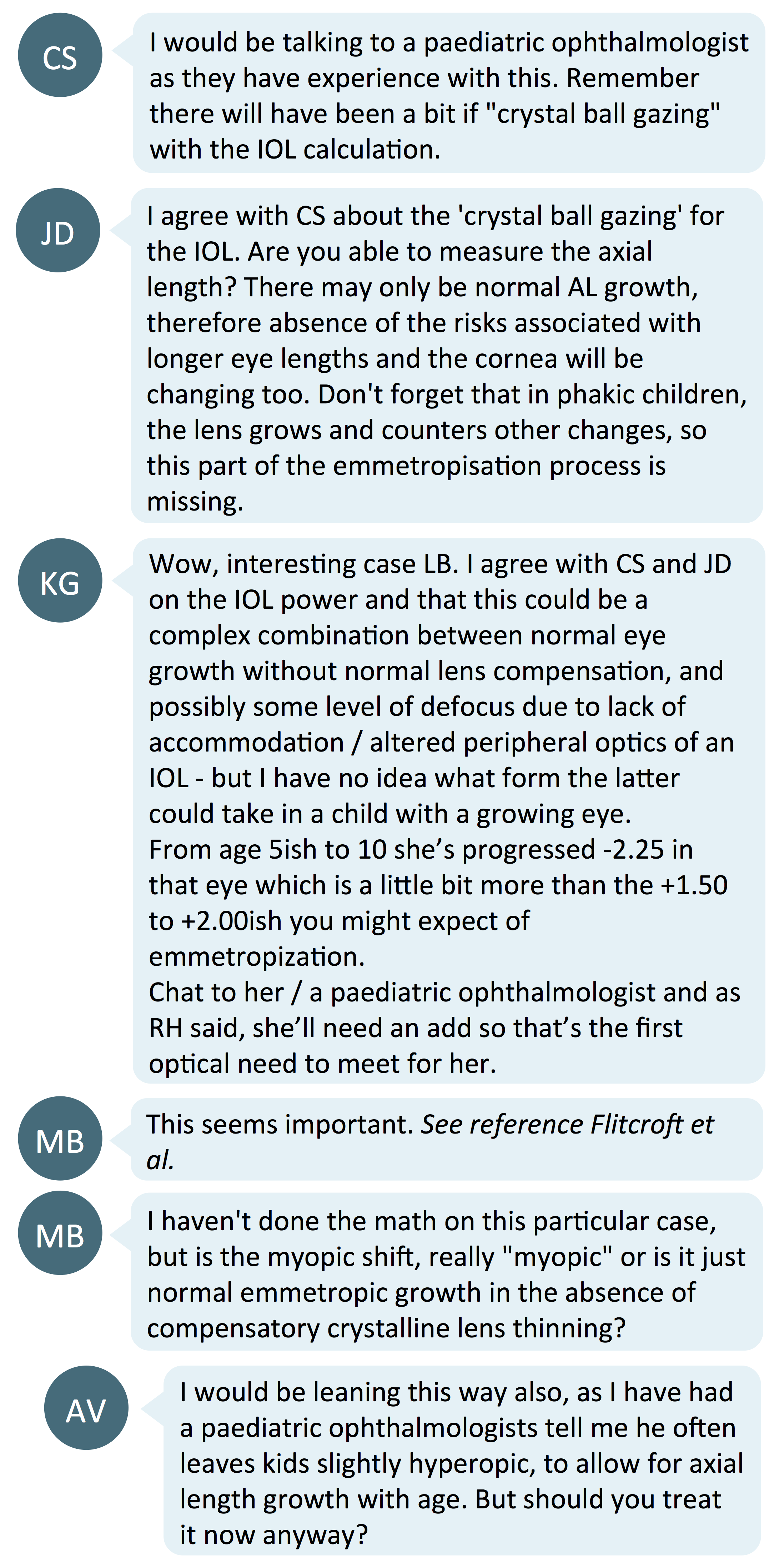
When a pseudophakic child shows a myopic change in refraction, should that be attributed to the normal axial elongation that occurs with typical eye growth in childhood, or is it a myopic (pathological) elongation?
The normal, phakic eye undergoes both passive emmetropization (that which occurs with normal eye growth) and active emmetropization (that which occurs in response to visual feedback in controlling the eye growth).
Passive emmetropization happens differently in pseudophakes, as they do not have the natural crystalline lens reducing in power to compensate for overall ocular power changes due to increasing axial length. Active emmetropization in pseudophakes is affected by several factors such as age of cataract development and age of surgery, which can lead to varying visual outcomes and influences the rate of axial elongation.1 Although normal emmetropization is disrupted in a pseudophake, Flitcroft showed that they have similar rate of growth in axial length and corneal flattening to the normal childhood eye.2
Typical myopic shifts in pseudophakic children
How much axial elongation is normal in a pseudophakic child? Plager et al followed children for a minimum of 4 years post cataract surgery. They showed that children who underwent cataract removal surgery at the age of 2-3, 6-7, 8-9 and 10-15 years had a mean myopic shift of 4.60D, 2.68D, 1.25D and 0.61D respectively.3 Crouch et al reports slightly higher degrees of myopic shifts in refraction.4 Hence, it is common for an ophthalmologist to choose an IOL power that is slightly hyperopic to account for this future myopic shift in refraction, instead of aiming for postoperative emmetropia as they would for adults.
As the child in this case had cataract surgery as a 2-year-old, one would expect her to have a myopic shift in refraction of about 5D in the 5 years post-op. We have clinical data indicating that in around 4.5 years, from age 6 to age 10, this child has progressed -2.25D in the right (normally sighted) eye and not progressed at all in the left (amblyopic) eye. While this represents more of a comparative loss of hyperopia in emmetropization across this age span, without the compensatory crystalline lens flattening it could be quite normal. Getting in touch with the child's ophthalmologist to ascertain the target post-op refraction could clarify the situation. Otherwise, obtaining axial length data may help confirm whether her axial length is within the normal range and undergoing typical elongation for her age.
Contact lenses versus spectacle lenses
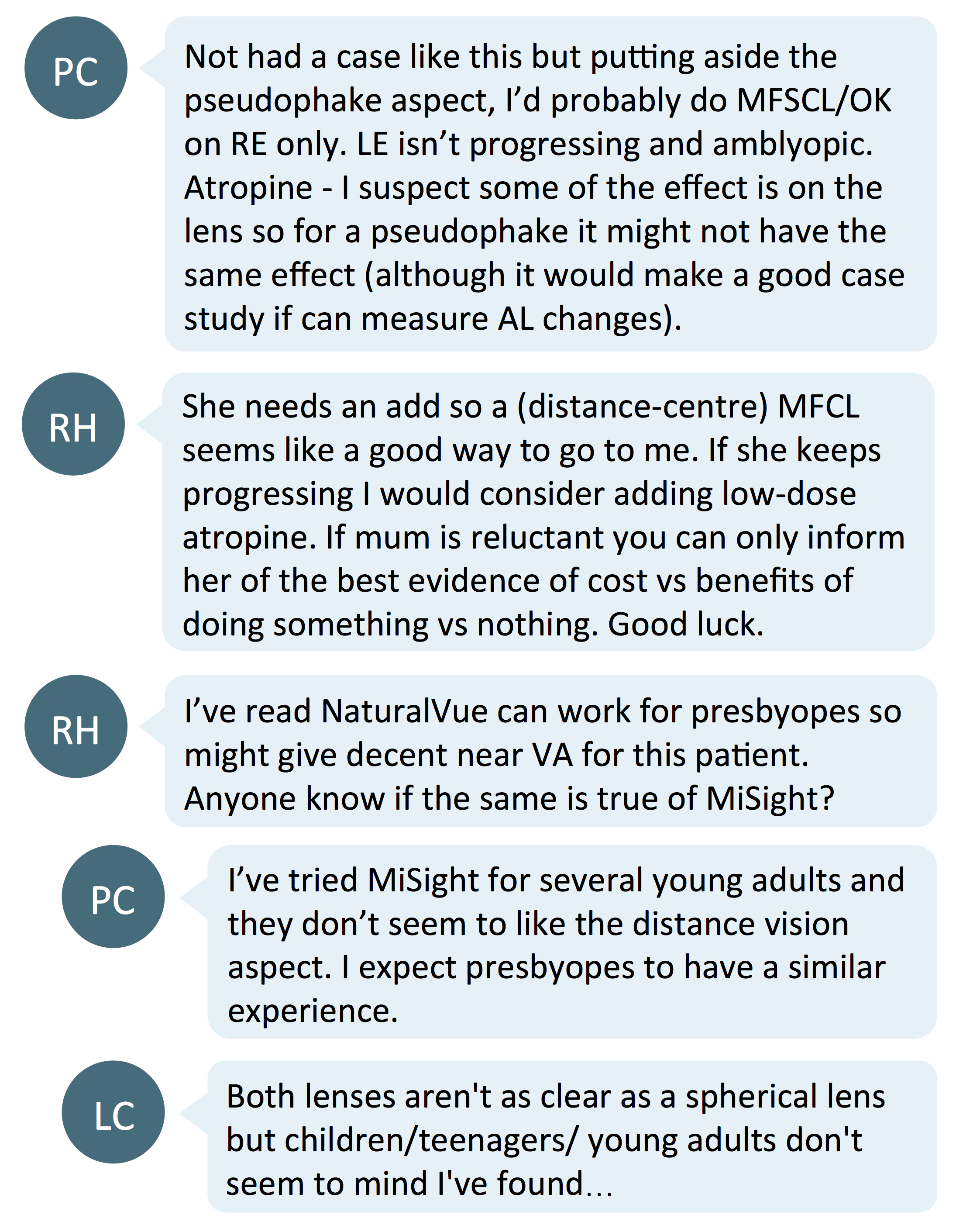
Due to the absence of a natural crystalline lens, a full near addition is necessary to allow for clear near vision. Commenters suggested prescribing multifocal or myopia controlling contact lenses, and/or low dose atropine to help in controlling myopia progression. However, the 'near add' effect provided by these contact lenses may not be as predictable as that provided by a spectacle lens add.5 Atropine could potentially affect near vision through pupil dilatation (it won't affect accommodation as it's not functional), but could be considered as the child is already wearing a full add to support near acuity.
Progressive or bifocal spectacle lenses are likely to be the best choice for pseudophakes of any refractive state. Given that this patient has no natural accommodation function, these spectacle lens options will give clear distance vision and a full powered, predictable add power for optimized near vision. If a myopia control effect is desired, data indicates that bifocal spectacle lenses will likely provide a strategy than progressive addition lenses - read more in Spectacle lenses for myopia control.
Does this pseudophakic child need myopia control?
Perhaps not. Her left, amblyopic eye is not progressing and her right, normally sighted eye may simply be exhibiting normal axial elongation in emmetropization. The myopic shift is then an exaggerated refractive outcome of emmetropization, due to the lack of compensating crystalline lens flattening.
This is an important case of atypical myopia where observation, especially with axial length measurement, is likely the most prudent course of management.
Take home messages:
- In a complex case like this with a prior history of ocular pathology and/or surgery, the refraction may not be as it seems. In childhood pseudophakia, 'myopia progression' could actually be normal emmetropization.
- The normal degree of change in myopic refraction differs depending on the age of cataract surgery, gender and ethnicity.1
- Deciding if a pseudophakic child requires myopia control can be complicated - measurement of axial length is key to determine if axial length is within the normal range and elongating at the typical rate for age. Informed consent in atypical cases of myopia is crucial. If parents and practitioner decide to proceed with myopia control, the child's need for a full add at near must be prioritized.

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.
This content is brought to you thanks to an unrestricted educational grant from
![]()
References
- Trivedi RH, Wilson Jr ME. Growth of aphakic and pseudophakic eyes. Pediatric cataract surgery: techniques, complications, and management. Philadelphia: Lippincott Williams & Wilkins. 2005:230-5.
- Flitcroft DI, Knight-Nanan D, Bowell R, Lanigan B, O’Keefe M. Intraocular lenses in children: changes in axial length, corneal curvature, and refraction. British Journal of Ophthalmology. 1999 Mar 1;83(3):265-9. (link)
- Crouch ER, Crouch Jr ER, Pressman SH. Prospective analysis of pediatric pseudophakia: myopic shift and postoperative outcomes. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2002 Oct 1;6(5):277-82. (link)
- Plager DA, Kipfer H, Sprunger DT, Sondhi N, Neely DE. Refractive change in pediatric pseudophakia: 6-year follow-up. Journal of Cataract & Refractive Surgery. 2002 May 1;28(5):810-5. (link)
- Kim E, Bakaraju R, Ehrmann K. Power Profiles of Commercial Multifocal Soft Contact Lenses, Optometry & Vision Science. 2017 Feb 94(2):183-96. (link)











