Note that this cover image does not represent any of the detail below - we just found it a visually pleasing representation of how we think of contrast in vision!
When myopia etiology is discussed, it is often explained using the peripheral defocus theory whereby peripheral hyperopic defocus signals the eye to elongate. However, the contrast theory contemplates a different stimulus for myopic eye growth: high contrast as a driver for myopia. The new SightGlass Vision DOT 0.2 lenses1 are designed to manipulate this physiological phenomenon and slow myopic progression by mildly reducing the contrast of imagery formed at the retina.
What is contrast theory in myopia?
The contrast theory for myopia hypothesises that high retinal contrast leads to overstimulation of the retina; this overstimulation is then thought to signal to the eye to continue growing. Low retinal contrast, on the other hand, signals the eye to slow or stop growing.1,2
How do genetic studies support the contrast theory?
A study investigating gene mutations in juvenile onset myopia found that cone photoreceptors - either the long-wavelength (red) or the medium-wavelength (green) cone opsin genes - were involved.3 Due to the mutations in these genes that affect the splicing process, the L or M cones tended to have a reduction in photopigment, causing an insensitivity to light.4
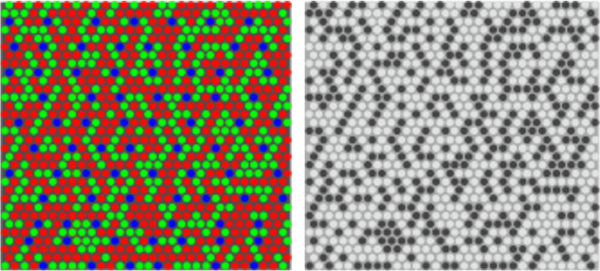
In the image above (supplied by SightGlass Vision), the left panel is a graphical representation of the human cone mosaic with the L, M and S (short-wavelength, blue) cones. The patients with myopia expressed the defective gene in either the L (red) or the M (green) cones. The L and M cones work together to give black and white vision - if red are functional and green were ignored, the mosaic of normal and mutant cones looks like the right panel.
Consider the retina, with its mosaic of various cone photoreceptors: mutations in one cone photoreceptor means there is a disparity between cone signalling between adjacent normal and affected cones. Cones without the mutation with normal amounts of photopigment will fire off as per normal. Cones with the mutation will not. This disparity in signalling between adjacent cones is detected by the bipolar cells and produces abnormally high contrast signalling (in terms of intensity and frequency) which stimulates eye growth. Greater photopigment deficit is correlated with higher degrees of myopia.4
Congenital Stationary Night Blindness does not have the gene mutation related to cone photopigment and yet is linked to myopia: this is thought to be because the mutations that do occur in this condition also cause abnormal contrast signalling at the retina as well, albeit through different means associated with the bipolar cells.5 Hence, the amount of contrast, rather than specific genetic mutations, are considered the driver of myopic progression.
Contrast theory in 'common' myopia
The abovementioned discovery provides a valuable insight into the patterns of activity in the retina that signal eye growth and myopia progression. So why does myopia still occur children without such genetic predisposing factors? Based on the contrast theory, this is linked to the high contrast near modern visual environment. Near work is well known to be associated with myopia progression.6 Contrast theory suggests that this near work disrupts emmetropization and causes myopia, by presenting a large amount of high contrast information across the retina.
This is because emmetropization adapted to occur outdoors. Children are born hyperopic. Their hyperopic eyes when outdoors are able to view distant scenery clearly and in high contrast; as the eyes lose their hyperopia, the contrast and detail in the distant scenery is also lost. This is an important feedback loop for the eye to determine when to stop the emmetropization process: high contrast signals the eye to continue growing; low contrast signals the eye to slow or stop.1,7
How is this different to the defocus theory in myopia?
Animal research has established both defocus and contrast visual signals influence ocular growth and refractive development.8 Other theories of myopia development, progression and control include the peripheral defocus9 and simultaneous defocus10 theories. What these theories have in common is that optical defocus is identified as a driver to eye growth: hyperopic defocus accelerates while myopic defocus slows eye growth. Defocus drives the eye to grow, or to stop growing, to find the point of focus.
Peripheral defocus is well understood, while the newer theory of simultaneous defocus can be pictured as on- or off-axis, where opposing defocus signals compete to signal eye growth10 Examples of myopia control treatments employing simultaneous defocus are the MiSight 1 day dual-focus contact lens, and the Defocus Incorporate Multiple Segments (DIMS) and Highly Aspherical Lenslet Target (H.A.L.T.) Technology spectacle lenses.
The image below (supplied by SightGlass Vision) indicates the visual impact of reduced contrast, blur and a combination of both.
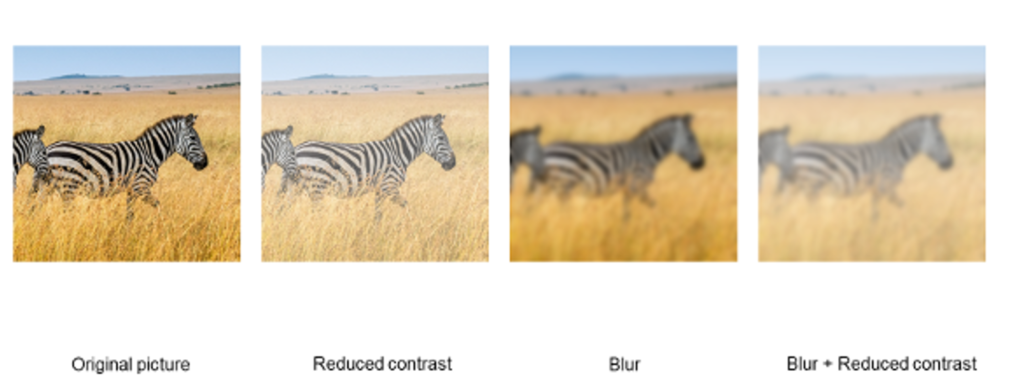
It is worth noting that research on DIMS and H.A.L.T. Technology spectacle lenses have shown that they too reduce contrast, although more so at mid-, high- and very-high spatial frequencies than uniformly. There are also small differences in the contrast sensitivity function produced by each lens type.11 It has also been suggested that contrast perception is instrumental in the detection of defocus.12 This indicates how contrast theory fits into the suite of mechanisms explored as part of myopia research.
Comparison of the same has not yet been undertaken with the DOT 0.2 lens, and no direct evaluation of myopia control efficacy has been undertaken across these three novel spectacle lens designs. It is difficult to compare the individual published performance of these three spectacle lenses as the study settings, ethnicity and age groups were very different.
Clinical application of the contrast theory
The SightGlass DOT lenses do not attempt to induce peripheral or simultaneous myopic defocus; rather, they slightly reduce peripheral contrast with microdots integrated across the lens. One-year clinical trial results indicate effective myopia control, supporting this newly described etiology of myopia development and control.1 Learn more about this lens via the links below.
Further reading
Important note: DOT lenses are currently not available in the US but are available in selected countries outside the US.

About Jeanne
Jeanne Saw is a clinical optometrist based in Sydney, Australia. She has worked as a research assistant with leading vision scientists, and has a keen interest in myopia control and professional education.
This content is brought to you thanks to an unrestricted educational grant from

References
- Rappon J, Chung C, Young G, Hunt C, Neitz J, Neitz M, Chalberg T. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomised controlled, efficacy and safety study (CYPRESS). Br J Ophthalmol. 2022 Sep 1:bjophthalmol-2021-321005. (link)
- Neitz M, Patterson SS, Neitz J. Photopigment genes, cones, and color update: disrupting the splicing code causes a diverse array of vision disorders. Curr Opin Behav Sci. 2019 Dec;30:60-66. (link)
- Winderickx J, Battisti L, Hibiya Y, Motulsky AG, Deeb SS. Haplotype diversity in the human red and green opsin genes: evidence for frequent sequence exchange in exon 3. Hum Mol Genet. 1993 Sep;2(9):1413-21.
- Neitz M, Wagner-Schuman M, Rowlan JS, Kuchenbecker JA, Neitz J. Insight from OPN1LW Gene Haplotypes into the Cause and Prevention of Myopia. Genes (Basel). 2022 May 25;13(6):942. (link)
- Musarella MA, Weleber RG, Murphey WH, et al. Assignment of the gene for complete X-linked congenital stationary night blindness (CSNB1) to Xp11.3. Genomics. 1989;5(4):727-737.
- Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ, Mitchell P. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008 Jul;49(7):2903-10.
- Neitz M, Wagner-Schuman M, Rowlan J et al. The End of Myopia,. Research Square.
- Troilo D, Smith EL 3rd, Nickla DL, Ashby R, Tkatchenko AV, Ostrin LA, Gawne TJ, Pardue MT, Summers JA, Kee CS, Schroedl F, Wahl S, Jones L. IMI - Report on Experimental Models of Emmetropization and Myopia. Invest Ophthalmol Vis Sci. 2019 Feb 28;60(3):M31-M88. (link)
- Smith EL 3rd. Prentice Award Lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011 Sep;88(9):1029-44. (link)
- Smith Iii EL, Arumugam B, Hung LF, She Z, Beach K, Sankaridurg P. Eccentricity-dependent effects of simultaneous competing defocus on emmetropization in infant rhesus monkeys. Vision Res. 2020 Dec;177:32-40. (link)
- Li X, Ding C, Li Y, Lim EW, Gao Y, Fermigier B, Yang A, Chen H, Bao J. Influence of Lenslet Configuration on Short-Term Visual Performance in Myopia Control Spectacle Lenses. Front Neurosci. 2021 May 25;15:667329. (link) [Link to Myopia Profile Science Review]
- Tkatchenko TV, Tkatchenko AV. Genome-wide analysis of retinal transcriptome reveals common genetic network underlying perception of contrast and optical defocus detection. BMC Med Genomics. 2021 Jun 9;14(1):153. (link)











