The most common parameter to monitor myopia progression is change in refractive error. However, as clinicians around the world become more proactive with prescribing myopia control strategies, axial length data becomes an increasingly valued piece in the clinical picture. If you aren't currently equipped with the appropriate equipment, how does one go about choosing an instrument to measure axial length?
Why is axial length measurement so important?
The main ‘why’ behind myopia control is to reduce the rate of axial length elongation. Whilst we can normally expect a direct correlation between axial length and refractive error, this is not always the case. A reduction in refractive progression does not always correlate to reduced axial length progression. Axial length measurements are also a valuable tool in monitoring the success of orthokeratology treatment in reducing myopic progression, as refraction is intentionally altered. It can also change one’s clinical management plan, such as in cases of a mismatch between myopia and axial length. An example of this is a low myope with long axial length, where a higher-than-expected risk for future pathology may lead to a more proactive management strategy.
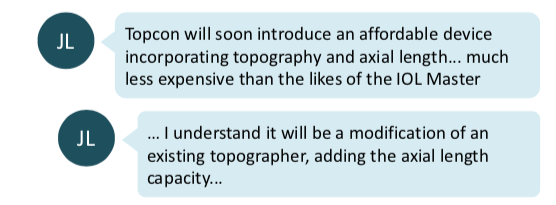
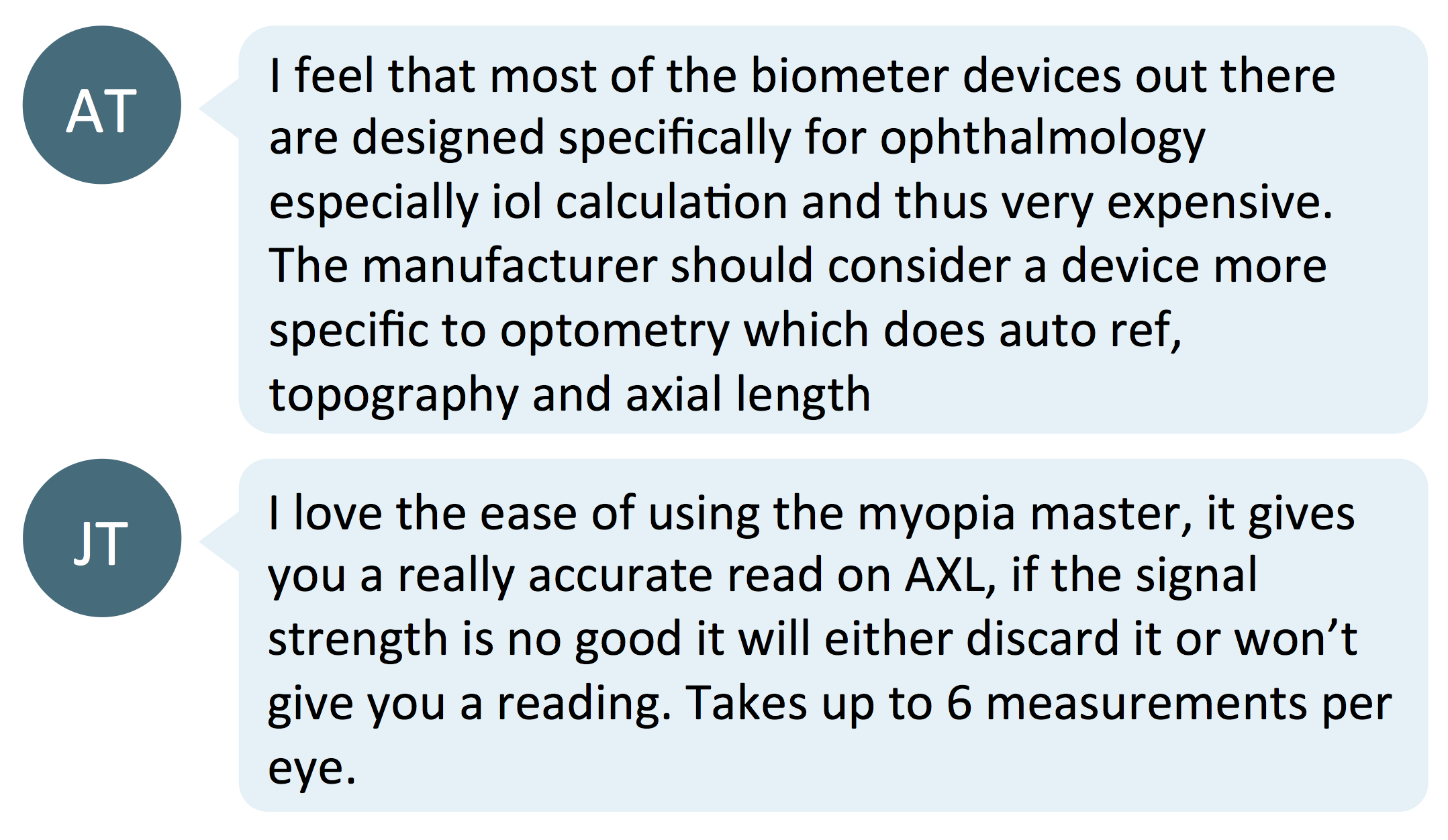
As biometric instruments are not yet traditionally used in optometric practices, practitioners may wonder which ones would be the most reliable to help monitor treatment success in myopia control. RM (link) and LF (link) asked the Myopia Profile Facebook community this precise question about choosing an instrument to measure axial length.
The community’s comments on their favourite instruments are summarised below.
Interferometry measurement instruments
Interferometry is a non-contact, optical biometry measure. Examples include the Zeiss IOLMaster, Haag-Streit LensStar and the OCULUS Pentacam AXL. These instruments have traditionally been used by ophthalmologists to measure corneal curvature and axial length and facilitate intraocular lens implant power calculations for cataract surgery. They have high repeatability and accuracy,1-5 and have been used in myopia control studies of orthokeratology,6-9 atropine8-10 and MiSight.11
Pros: high repeatability and accuracy, reliable, non-contact measurement technique
Cons: single function instrument, typically quite expensive for primary eye care
A-scan Ultrasonography
A-scan ultrasound biometers have been used in several myopia control research studies to monitor axial length – typically older studies on bifocal and progressive spectacle lenses12-14 and atropine.14-15 Ultrasound measurement requires anaesthesia and corneal applanation, so children may be intimidated by the drop instillation and/or the probe’s proximity to the eye. There is a steeper learning curve in getting consistent and repeatable measurements due to applanation pressure and is dependent on the operator.
Interferometry versus ultrasound - which is more accurate?
In application to myopia, the IMI Clinical Trials and Instrumentation report explains that ultrasonography is limited in resolution to about 0.30D, whereas interferometry measurements have resolution of around 0.03D, making this technique an order of magnitude better as a measure of myopia progression. Cycloplegic autorefraction, by comparison, has a repeatability of ±0.21D.16
In orthokeratology lens wear, a study comparing ultrasound and interferometry (IOLMaster) measurements of axial length found the latter to be more repeatable. The authors concluded that "measurements with the IOLMaster can replace the measurements from the two A‐scan ultrasonic biometers used, however, the reverse is not true."17
Measurement of axial length with non-contact interferometry instruments is more accurate and repeatable than by A-scan ultrasound biometry.
Combination instruments
There are also a range of instruments that combine several functions in one, which offers increased convenience for the practitioner and patient. Some are designed specifically for myopia management, with additional testing capacity and software outputs to streamline both testing and clinical communication.
Optopol REVO
Axial length + OCT. The Optopol REVO takes axial length measurement by using OCT imaging across the entire length of the eye. It has good axial length repeatability, and its measurements are in good agreement with those obtained on the IOLMaster.18
Topcon ALADDIN and MYAH
Axial length + corneal topography + pupillometry + dry eye assessment + progression reports. Topcon has released the Aladdin and the Myah (known as Aladdin-M in USA), both of which measure axial length and corneal topography. The Myah / Aladdin-M also includes pupillometry and dry eye assessment capabilities. Reporting to track progression include refraction (extra input required) and axial length charts. The Topcon technology uses non-contact, interferometry measurement of axial length, and has been demonstrated to be comparable to the IOLMaster.19
OCULUS Myopia Master
Axial length + keratometry + autorefraction + progression reports + risk factor analysis outputs. The OCULUS Myopia Master is a multi-function instrument, featuring autorefraction, axial length measurement and keratometry. It also has software developed in cooperation with the Brien Holden Vision Institute that provides axial length growth chart outputs and provides risk factor assessment to support clinical communication. The take-home report for parents provides the results, and also provides support on understanding myopia. The report can be printed or sent via email, together with the date for the next consultation, directly from the software. The OCULUS technology uses non-contact, interferometry measurement of axial length, which has been demonstrated to be in agreement with the IOLMaster.20 Since the Myopia Master was designed especially for the Optometrist, the combination of measurements provide utility for all patients, not just myopia management, through the Autorefractor and Keratometer functions.
Pros: repeatable and accurate, non-contact measurement, multi-functional, space- and time-saving, more affordable than single-function interferometry instruments, designed for primary eye care
Cons: none come to mind!
Take home messages:
- There are many considerations in choosing an instrument to measure axial length, including affordability, size and ease of use.
- Interferometry measurement instruments are more accurate than ultrasound measurements, but have traditionally been used by ophthalmology and been expensive for primary eye care.
- Multiple function instruments which employ interferometry, especially those specifically designed for myopia, provide useful clinical functionality and affordability for primary eye care practitioners, as well as tools for reporting and clinical communication.

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.
This content is brought to you thanks to an unrestricted educational grant from
References:
- Lam AK, Chan R, Pang PC. The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster™. Ophthalmic and Physiological Optics. 2001 Nov;21(6):477-83. (link)
- Wang XG, Dong J, Pu YL, Liu HJ, Wu Q. Comparison axial length measurements from three biometric instruments in high myopia. International journal of ophthalmology. 2016;9(6):876. (link)
- Németh J, Fekete O, Pesztenlehrer N. Optical and ultrasound measurement of axial length and anterior chamber depth for intraocular lens power calculation. Journal of Cataract & Refractive Surgery. 2003 Jan 1;29(1):85-8. (link)
- Iqbal F, Khan HA. Comparative analysis of axial length measurement using partial coherence interferometry and clinical ultrasound. Adv Ophthalmol Vis Syst. 2019;9(1):11-3. (link)
- Epitropoulos A. Axial length measurement acquisition rates of two optical biometers in cataractous eyes. Clinical Ophthalmology (Auckland, NZ). 2014;8:1369. (link)
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Investigative ophthalmology & visual science. 2012 Jul 1;53(8):5060-5. (link)
- Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Investigative ophthalmology & visual science. 2012 Jun 1;53(7):3913-9. (link)
- Kinoshita N, Konno Y, Hamada N, Kanda Y, Shimmura-Tomita M, Kakehashi A. Additive effects of orthokeratology and atropine 0.01% ophthalmic solution in slowing axial elongation in children with myopia: first year results. Japanese journal of ophthalmology. 2018 Sep 1;62(5):544-53. (link)
- Lin HJ, Wan L, Tsai FJ, Tsai YY, Chen LA, Tsai AL, Huang YC. Overnight orthokeratology is comparable with atropine in controlling myopia. BMC ophthalmology. 2014 Dec 1;14(1):40. (link)
- Polling JR, Kok RG, Tideman JW, Meskat B, Klaver CC. Effectiveness study of atropine for progressive myopia in Europeans. Eye. 2016 Jul;30(7):998-1004. (link)
- Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year randomized clinical trial of MiSight lenses for myopia control. Optometry and Vision Science. 2019 Aug 1;96(8):556-67. (link)
- Cheng D, Woo GC, Drobe B, Schmid KL. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: three-year results of a randomized clinical trial. JAMA ophthalmology. 2014 Mar 1;132(3):258-64. (link)
- Edwards MH, Li RW, Lam CS, Lew JK, Yu BS. The Hong Kong progressive lens myopia control study: study design and main findings. Investigative ophthalmology & visual science. 2002 Sep 1;43(9):2852-8. (link)
- Shih YF, Hsiao CK, Chen CJ, Chang CW, Hung PT, Lin LL. An intervention trial on efficacy of atropine and multi‐focal glasses in controlling myopic progression. Acta Ophthalmologica Scandinavica. 2001 Jun;79(3):233-6. (link)
- Fan DS, Lam DS, Chan CK, Fan AH, Cheung EY, Rao SK. Topical atropine in retarding myopic progression and axial length growth in children with moderate to severe myopia: a pilot study. Japanese journal of ophthalmology. 2007 Jan 1;51(1):27-33. (link)
- Moore KE, Berntsen DA. Central and peripheral autorefraction repeatability in normal eyes. Optom Vis Sci. 2014;91(9):1106-12. (link)
- Chan B, Cho P, Cheung SW. Repeatability and agreement of two A‐scan ultrasonic biometers and IOLMaster in non‐orthokeratology subjects and post‐orthokeratology children. Clinical and Experimental Optometry. 2006 May;89(3):160-8. (link)
- Sikorski BL, Suchon P. OCT Biometry (B-OCT): A New Method for Measuring Ocular Axial Dimensions. Journal of ophthalmology. 2019 Aug 14;2019. (link)
- Mandal P, Berrow EJ, Naroo SA, Wolffsohn JS, Uthoff D, Holland D, Shah S. Validity and repeatability of the Aladdin ocular biometer. Br J Ophthalmol. 2014 Feb;98(2):256-8. (link)
- Sel S, Stange J, Kaiser D, Kiraly L. Repeatability and agreement of Scheimpflug-based and swept-source optical biometry measurements. Cont Lens Anterior Eye. 2017 Oct;40(5):318-322. (link)











