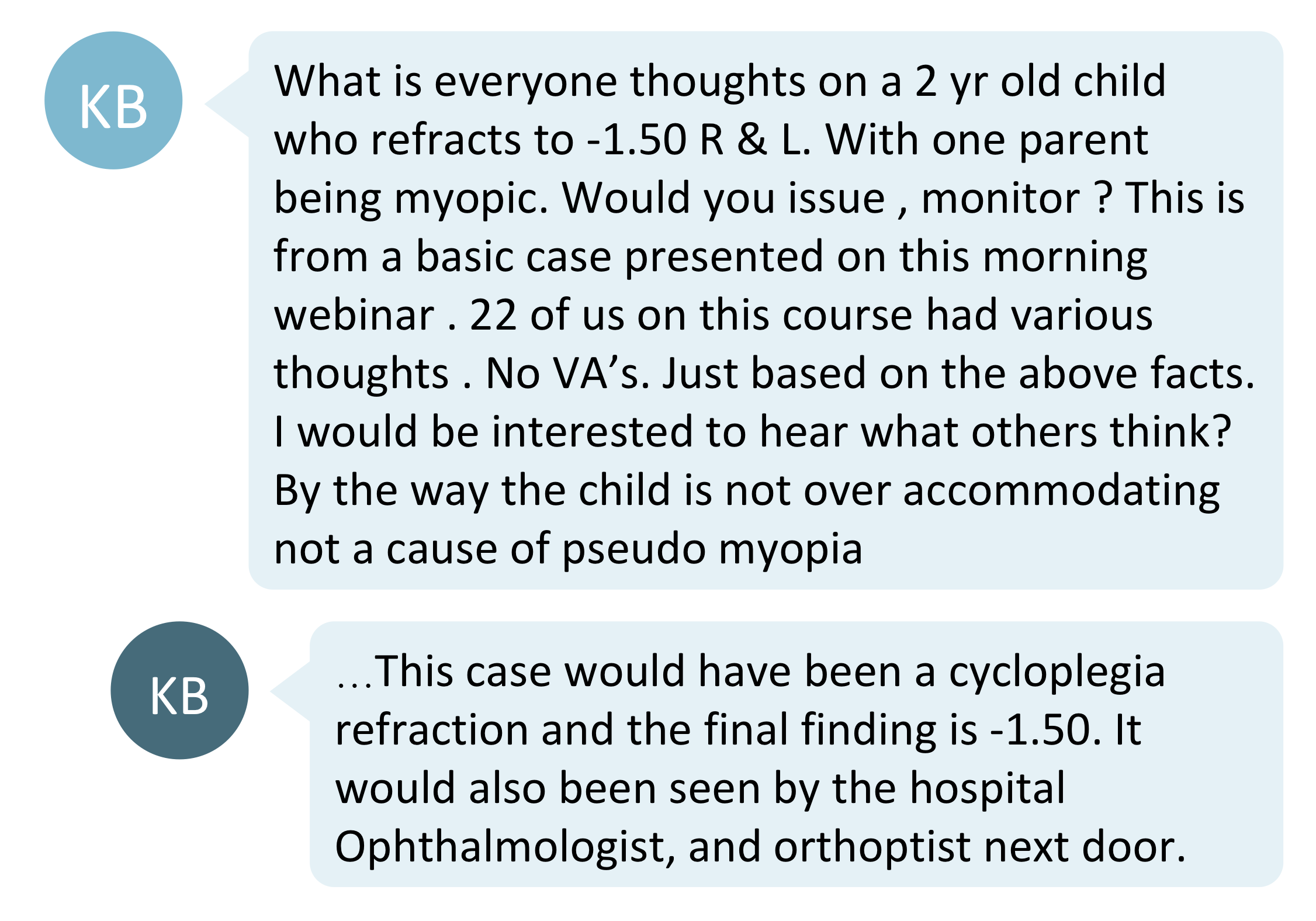
Would you prescribe glasses for a young child with mild myopia? Is myopia control beneficial for a toddler? What are the key clinical considerations? KB shared an interesting case about a two-year-old child with -1.50D of myopia in the Myopia Profile Facebook group.
What are the considerations?
Limited research and patient information


Currently, there are no studies about the likelihood or typical rate of myopia progression for a two-year-old child. Without that information, we cannot justify with certainty that myopia control is required or would be beneficial at that age.
While commenters also highlighted that we lack other useful information such as the child’s axial length and binocular vision status, which could influence one’s management, there is question of how much value this provides in a child so young. The key management strategies at this age would be to ensure clear visual input to avoid amblyopia. If the child also had significant astigmatism or strabismus this would make the management simpler - vision correction and more active management would be required.
Even though the myopia is low, it is unusual to be myopic at such a young age - therefore it is critical to consider referring the child to an ophthalmologist to rule out any systemic co-morbidities. The mandatory nature of referral for a toddler with low myopia will depend on the scope of practice of primary eye care in your country. Once this care pathway has been satisfied according to your specific professional requirements in your country, it is likely that management of optical correction will fall back to the primary eye care practitioner. It is important to note that the case presented mentioned that the child had already seen an ophthalmologist, and the focus was on how to manage the refraction – to correct or not?
Should we prescribe optical correction?
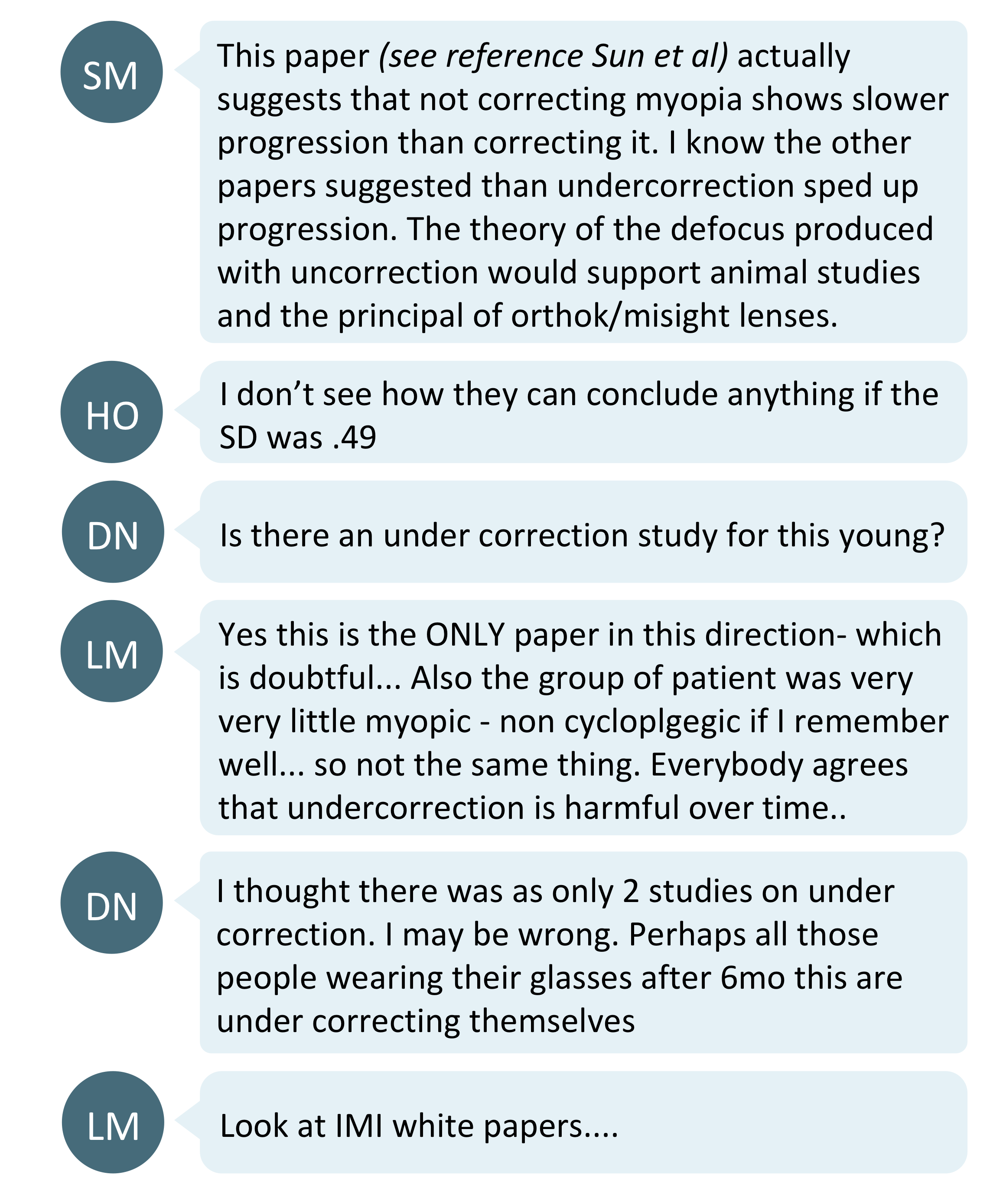
The community's opinions were split about the management of this child. The minority said they would prescribe glasses whilst the rest would choose to monitor the child first.
'Time to treat' group
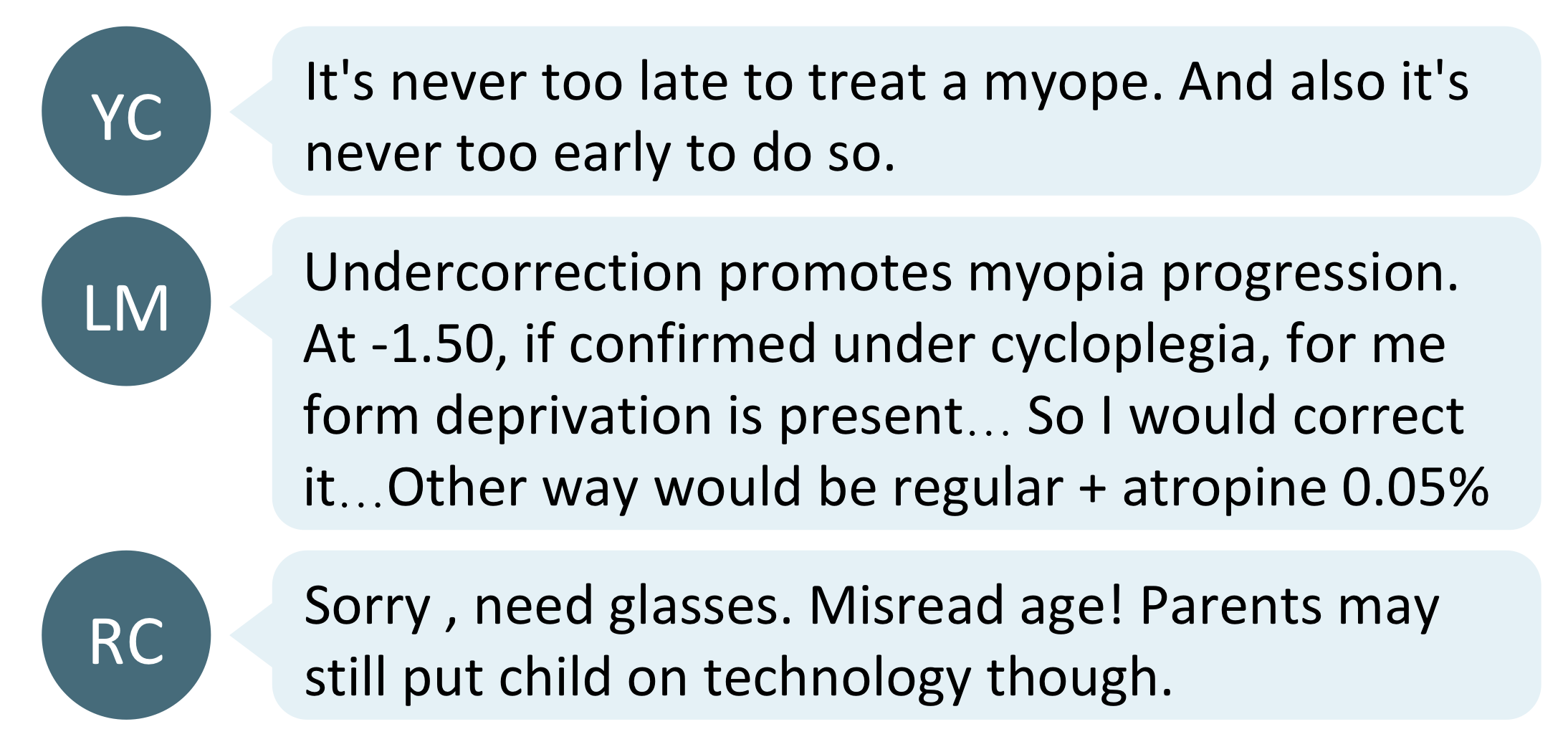
The rationale behind prescribing glasses now was to avoid under-correction, which has been suggested to be linked to increased myopia progression as highlighted in the discussions below. However it's important to note that children this young are not typically included in myopia control studies, so the influence of undercorrection on a two-year-old is unknown. The ensuing discussion highlighted that there is some conjecture on undercorrection being harmful in myopia, and how well the studies apply to this patient.
What the research says:
- Sun et al showed that having no myopia correction slows myopia progression.1
- Li et al suggested full correction and undercorrection of myopia show the same rate of myopia progression.2
- Adler et al, Chung et al and Vasudevanet al showed undercorrection promote myopia progression.3-5
The youngest subjects in all these studies were school-aged children, with vastly different visual needs and tasks to a two-year-old toddler. Hence, it would be difficult to extrapolate these conclusions for this child. To read more on undercorrection and un-correction, check out this research blog which describes a recent meta-analysis paper on the topic. The conclusion of this meta-analysis was that undercorrection doesn't appear to be beneficial in myopia and is unlikely to be suitable as an intentional clinical management strategy.
'Time to monitor' group
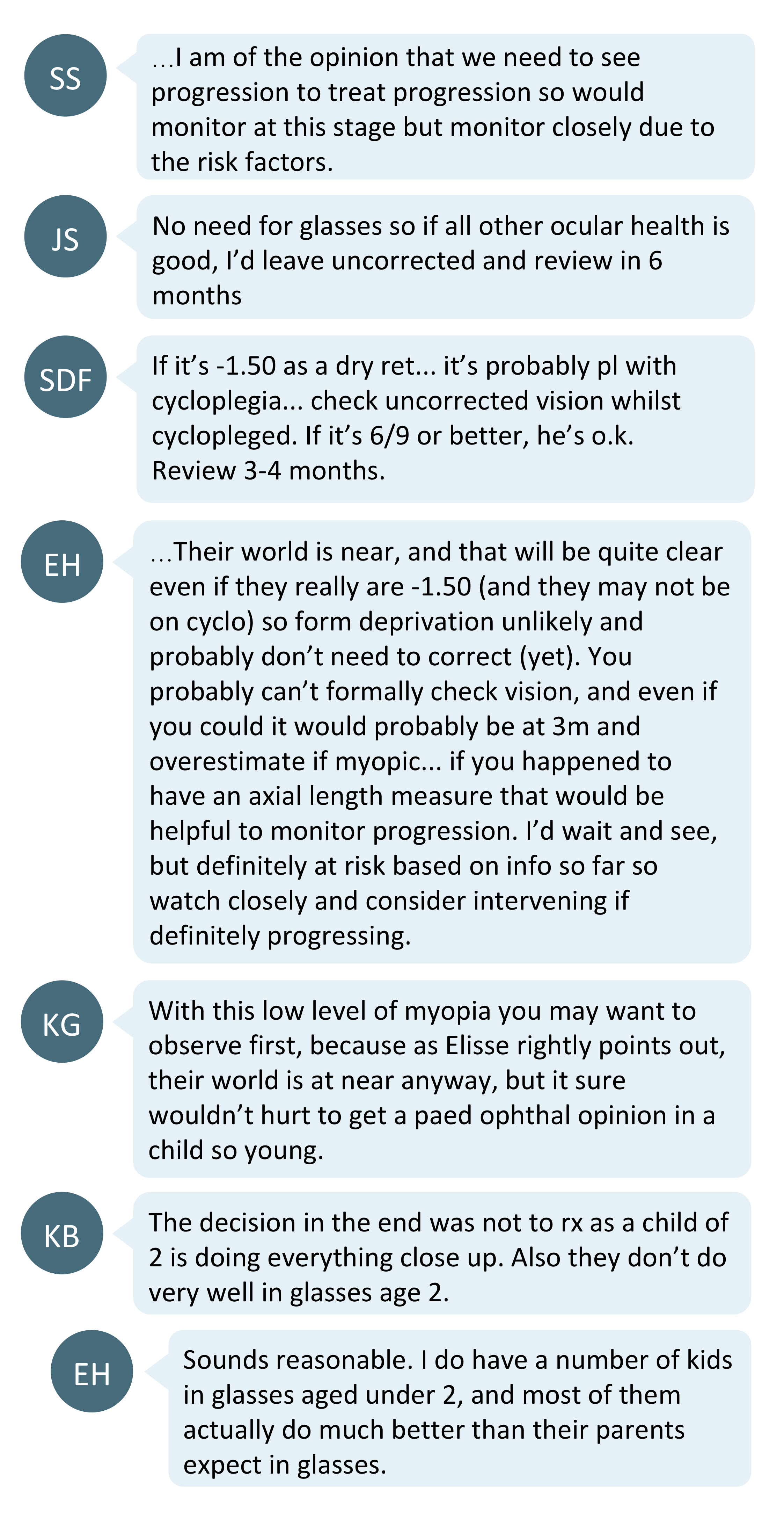
Most commenters suggested monitoring the child first due to the lack of myopia control research for this age group. The visual world of children at this age is mostly close up. Thus, not correcting this low level of myopia is highly unlikely to lead to form deprivation amblyopia as the world at close distances is entirely clear for this child.
However, monitoring the child’s myopic progression is important. And whilst not everybody would necessarily prescribe glasses at this stage, documented progression would be a stronger indicator for intervention. It is also worth highlighting again that, despite the low myopia, the community did comment that seeking an opinion of a paediatric ophthalmologist would be important. In the case presented, the child had already seen an ophthalmologist. Whether this is mandatory or not will depend on the scope of practice in your country for managing children in this age group.
In looking to consensus on prescribing for toddlers, the American Academy of Ophthalmology’s Preferred Practice Patterns for Pediatric Eye Evaluations (2017) advises correction for myopia of 3D or more at age 2 to <3 years. (Table 3) This data is given with a note that “these values were generated by consensus and are based solely on professional experience and clinical impressions because there are no scientifically rigorous published data for guidance. The exact values are unknown and may differ among age groups; they are presented as general guidelines that should be tailored to the individual child.” A research review published in 2011 recommended that for myopia without anisometropia or astigmatism, children 1-2 years of age be corrected for more than 2D of myopia once walking; from 2-4 years of age be corrected from 1.50D of myopia if it improves function. In both cases it’s suggested to reduce the refraction by 0.50-1.00D for emmetropization until age 4. You can read this open access paper here. It appears from research and consensus that it may be appropriate to not prescribe a correction in this case, based on this first presentation.
Managing the visual environment

Regardless of whether one decides to correct this level of myopia at this stage, the consensus is that increasing time outside and reducing near work is an important part of managing this child.
Research shows that sufficient outdoor time can slow the onset of myopia, although there is conjecture about its role in reducing progression after myopia onset.6 Eyecare practitioners can recommend children spend at least 90 minutes a day outdoors. It is important to still encourage sun safety whilst doing this - that is to wear hats and sunglasses.
Excess near work is linked to increased rates of myopia progression,7 and according to the American Academy of Pediatrics and Australian Government Department of Health, screen time is not recommended in children under the age of two, for a variety of developmental reasons - not just visual. Children aged 2-5 years are suggested to have a maximum of one hour of screen time per day. For these weblinks and a reference to give parents, head to the My Kids Vision blog entitled Close Work and Screen Time.
Take home messages:
- Children under age 10 with high myopia (more than 5-6D) should always be referred and/or co-managed with paediatric ophthalmology. This child is not a high myope but is very young - consideration of seeking a paediatric ophthalmologist’s opinion on management is critical in cases of very young myopes. It may be mandatory in your country, depending on the scope of primary eye care practice. In this case, it was noted that the child had already had ophthalmological review, and the focus was on refractive management.
- Prescribing glasses isn’t always the first necessary step when you are presented with the very young myope. Considering the visual needs of the child will aid that decision, and the research and consensus guidelines do support not prescribing, and observing, in this case. Very young children have a closer ‘world’ of visual tasks, and the key imperative at this age is to avoid amblyogenesis.
- Regardless of age, the importance of outdoor time and managing near work time should be discussed with parents. Resources for parents are available on the My Kids Vision website.
Further reading on prescribing for young children

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.
This content is brought to you thanks to an unrestricted educational grant from
![]()
References:
- Sun YY, Li SM, Li SY, Kang MT, Liu LR, Meng B, Zhang FJ, Millodot M, Wang N. Effect of uncorrection versus full correction on myopia progression in 12-year-old children. Graefe's Archive for Clinical and Experimental Ophthalmology. 2017 Jan 1;255(1):189-195. (link)
- Li SY, Li SM, Zhou YH, Liu LR, Li H, Kang MT, Zhan SY, Wang N, Millodot M. Effect of undercorrection on myopia progression in 12-year-old children. Graefe's Archive for Clinical and Experimental Ophthalmology. 2015 Aug 1;253(8):1363-8. (link)
- Adler D, Millodot M. The possible effect of undercorrection on myopic progression in children. Clinical and Experimental Optometry. 2006 Sep;89(5):315-21. (link)
- Chung K, Mohidin N, O’Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision research. 2002 Oct 1;42(22):2555-9. (link)
- Vasudevan B, Esposito C, Peterson C, Coronado C, Ciuffreda KJ. Under-correction of human myopia–is it myopigenic?: a retrospective analysis of clinical refraction data. Journal of optometry. 2014 Jul 1;7(3):147-52. (link)
- Cao K, Wan Y, Yusufu M, Wang N. Significance of Outdoor Time for Myopia Prevention: A Systematic Review and Meta-Analysis Based on Randomized Controlled Trials. Ophthalmic research. 2020;63(2):97-105. (link)
- Huang HM, Chang DS, Wu PC. The association between near work activities and myopia in children—a systematic review and meta-analysis. PloS one. 2015 Oct 20;10(10):e0140419. (link)











