PC posed a question regarding the acceptable amount of over-correction to incorporate in an OrthoK prescription to allow for good end-of-day vision in this post. Here’s what the community said:
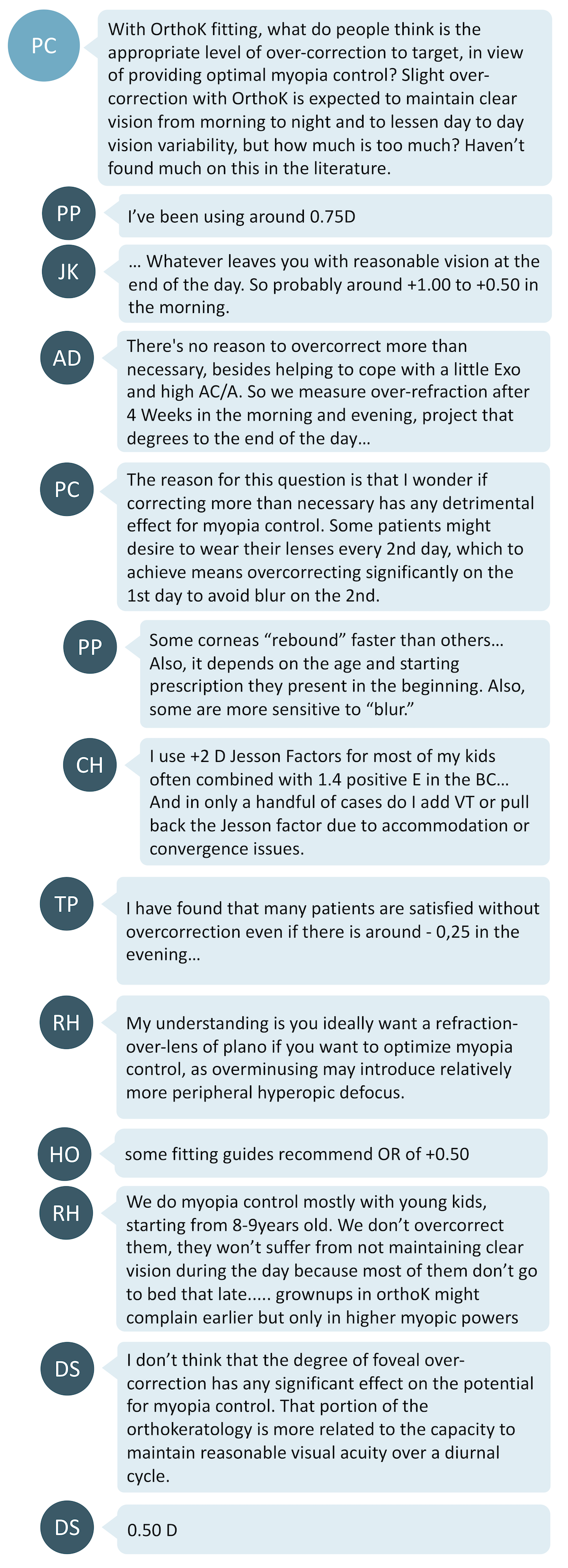
What are the considerations?
Reasons for over-correcting:
- General consensus was to over-correct by 0.50D to 1.00D. However, this number may vary between patients, depending on how fast a cornea ‘rebounds’.
- Sometimes, over-correcting may help in a person with high exophoria or AC/A ratio
- One can consider measuring over-refraction after 4 weeks of wear in the morning and evening to work out the perfect over-correction
- Some kids may prefer to wear the lenses every 2nd night but that may mean significant over-correction
- Some may be more sensitive to blur than others so over-correction will help guarantee clear end-of-day vision.
Reasons for not over-correcting:
- May not be particularly necessary as any blur at the end of the day is minimal, especially since younger kids will tend to have shorter waking hours (earlier bedtimes) than for the same consideration in adults
- A plano over-refraction may be ideal, in the case that too much over-correction (manifest hyperopia) could potentially reduce the relative peripheral myopia desired from OrthoK treatment.
What the research tells us:
- Mountford et al1 showed that the degree of regression during day-time hours is about 0.50-0.75D on average after 90 days of wear.
- However, Chan et al2 showed that the conventional 0.75D over-correction was insufficient for full myopia correction to last through the day for some patients.
- Gardiner et al3 showed that the amount of regression increases with higher amounts of baseline myopia. For example, a -4.00D myope regresses by about 1.00D at the end of the day on average.
- Lau et al4 hypothesised that a higher amount of over-correction (study was up to 1.75D) may actually potentially improve the myopia control effect due to increased amounts of high order aberrations (HOAs) that have been suggested to play a part in reduction of axial elongation.5 However, increased HOAs may lead to poor low-light visual performance.
- A clinical trial was completed in late 2019 which investigated OK fitting with a 'conventional compression factor' (0.50-0.75D over-correction target) compared to a matched group wearing OK with an 'increased compression factor' (1.50-1.75D over-correction target). The intended outcome was to measure any difference in myopia correction and control effects between the two lens fitting approaches. So far, preliminary findings have been reported indicating that the increased compression factor of 1D achieved around 0.30D additional refractive correction on average, after one month of wear, but unaided VA results were not significantly different between the groups.6 Any relationship to the myopia control effect will likely be reported in future.
- There have been no studies equating the amount of over-correction in OrthoK with the shift in peripheral refraction, and how this relates to myopia control efficacy. While it makes logical sense that too much over-correction could influence the optics of OrthoK, until we understand more about how this could relate to the myopia control effect, the main concern is to ensure good vision for our OK wearing patients throughout the day. This includes good vision at near, which could potentially be influenced by too much over-correction (manifest hyperopia).
Take home messages:
- Most contact lens companies already include approximately 0.50-0.75D of over-correction to account for regression during the day and this may be sufficient for most patients. For patients who do not reach full correction, an 'increased compression factor', or targeted higher over-correction, will be required.
- It is prudent to check the patient’s end-of-day over-refraction after 4 weeks of wear, as it will give you a better idea of the patient’s level of vision at that time and adjustments can be made if they are bothered by poor end-of-day vision.
- Incorporating a larger amount of over-correction than the lab’s standard 0.50-0.75D still remains a valid option to ensure good end-of-day acuity, provided it isn't too much to affect comfortable near vision.
- The relationship between over-correction and OrthoK's myopia control effect has not yet been established, but a clinical trial completed in late 2019 may soon provide data on this question.

About Kimberley
Kimberley Ngu is a clinical optometrist from Perth, Australia, with experience in patient education programs, having practiced in both Australia and Singapore.

About Connie
Connie Gan is a clinical optometrist from Kedah, Malaysia, who provides comprehensive vision care for children and runs the myopia management service in her clinical practice.
This content is brought to you thanks to an unrestricted educational grant from
![]()
References
- Mountford J. Retention and regression of orthokeratology with time. International Contact Lens Clinics 1998;25(2):60-64 (link)
- Chan B, Cho P, Mountford J. The validity of the Jessen formula in overnight orthokeratology: a retrospective study. Ophthalmic Physiol Opt 2008; 28: 265–268 (link)
- Gardiner HK, Leong MA, Gundel RE. Quantifying regression with orthokeratology. Contact Lens Spectrum 2005;20:40-43 (link)
- Lau JK, Vincent SJ, Cheung SW, Cho P. The influence of orthokeratology compression factor on ocular higher‐order aberrations. Clinical and Experimental Optometry 2020;103(1):123-128 (link)
- Lau JK, Vincent SJ, Cheung SW, Cho P. Higher order aberrations and axial elongation in myopic children treated with orthokeratology. Investigative Ophthalmology & Visual Science 2020;61(2):22 (link)
- Wan K, Lau JK, Cheung SW. Cho P. Orthokeratology with increased compression factor (OKIC): study design and preliminary results. BMJ Open Ophthalmology 2020;5:e000345 (link)











