This year, the annual Association for Research in Vision and Ophthalmology (ARVO) was held in Vancover 2019 from April 28th to May 2nd. Check out the Myopia Profile Facebook group for individual live posts, but here is a summary of the fabulous new research presented at the conference. Click on the headings for more information and a link to the presentation abstract. You'll find links to Part 2 and Part 3 of the ARVO latest at the end of this blog.

Get ready for your views to be changed on how we discuss efficacy of myopia treatments. Here’s Xu Cheng (Cathy), Noel Brennan and Mark Bullimore presenting their important work on understanding whether efficacy is relative (a percentage) or absolute. Analysing 93 datasets of a variety of treatment vs control, it revealed the typical trend of efficacy being much higher in the initial year compared to following years. This is why shorter studies frequently show higher % treatment effects.

This shows trend lines for numerous OrthoK, soft multifocal CLs and bifocal / progressive spectacle treatments. When the big initial response and reduced response in subsequent years is plotted, there’s a pretty clear picture that the treatment appears to plateau out to an absolute effect, of around 0.45mm (in OrthoK) or 1D (bifocal specs). Look how it also shows similarity between the treatments.
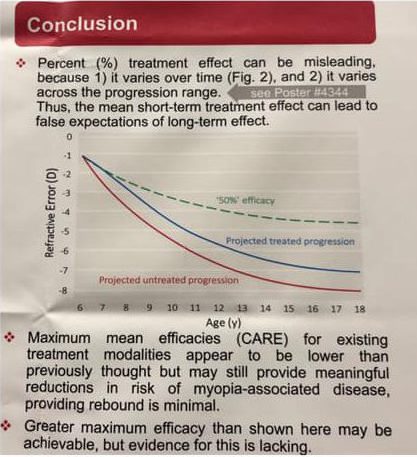
Now look at the conclusions and accompanying chart. The authors propose that it may not be appropriate to extrapolate something like 50% across many years of potential childhood progression - they’ve coined the term Cumulative Absolute Reduction in axial Elongation; the ‘CARE’ factor!
These guys aren’t trying to depress you about the value of myopia control, simply to ensure an appropriate and evidence based way to understand efficacy and interpret studies. So is it worth it for what could amount to perhaps only 0.45mm or 1D of myopia reduction? The answer is yes! More work by Mark and Noel presented at AAO2018 has shown a reduction in the risk of myopic maculopathy of 40% for each 1D reduction in myopia. (Check out the blog post on “Why 1D matters” for more info).
Divya Jagadeesh and colleagues at UNSW and BHVI evaluated fundus images in 56 eyes of 28 myopic children at baseline and after 12 months. Using semi-automated analysis, they found a multifactorial model including fovea-to-disc distance, disc tilt, temporal crescent, vessel angles to the disc and fundus tesselations which could account for up to 63% of variance in axial length.
The clinical relevance? In future, perhaps the work of these clever people will lead to development of a computerised fundus image analysis which can predict myopia progression to guide our interventions, or even to ‘measure’ axial length from fundus features.
Yee Ling Wong and colleagues in Singapore examined the 6 year incidence of myopic macular degeneration (MMD) in more than 6,000 adults over 40 years of age, showing a low incidence of MMD (1.7%) and relatively low progression (17.3%) in those with existing MMD. More severe MMD, as graded by the META-PM system, was at greater risk of progression. Fundus tesselation at baseline was the strongest predictor of future MMD. Older age, higher myopia and longer axial length were associated with incidence (new onset) of MMD, while age wasn’t a factor in likelihood of MMD progression - myopia and axial length were.
These numbers may seem low but the impact is larger. Mild MMD affects best corrected visual acuity and function, while severe MMD was found to affect reading, mobility and emotional quality of life scores.
Just as we’re diligent to avoid the disaster of end stage glaucoma with early intervention, this is more indication of the importance of early intervention in progressive childhood and high adult myopia to avoid the disaster of severe MMD.
Seang-Mei Saw, Zhi-Dah Soh and their colleagues compared the three year myopia progression rates of children in Finland and Singapore. Matched datasets of low myopic children (-0.50 to -3.00) were analysed with intriguing results.
Finish and Singaporean myopes aged 9-13 years at baseline had similar amounts of progression during the study, around -1.50D. Younger Singaporean children, aged 7-8 years, progressed -2.5D in three years. These results indicate that the younger age is related to both duration and speed of progression, and being a low myope at 7-8 is a risk factor for significant amounts of progression.
Parental surveys of near work and outdoor time per day showed that;
- Near work: Finland = 1.8 hours, Singapore = 3.5 hours
- Outdoor time: Finland = 3.5 hours, Singapore = 0.5 hours
What can we interpret from these visual environment statistics when their myopia progression was the same? Another session showed we can’t entirely write off the influence of outdoor time on myopia progression; it’s agreed that outdoor time has a significant influence on delaying myopia onset, but there is conjecture on progression even though there is some evidence. This Finland-Singapore comparison likely shows us that while myopia is no doubt incredibly complex, some of its factors are global.
Chinese eye exercises don’t influence myopia progression. Now upon reading that last sentence you may scoff and guffaw and even roll your eyes (as millions of Chinese children are doing daily) but this is a public health issue in China. As the abstract states; “Daily eye exercises massaging periocular acupuncture pressure points have been part of China’s national vision care policy in schools for around 50 years”. There is also a real issue with children suffering uncorrected myopia due to the persistent belief that glasses weaken the eyes. Hence this was a study which needed to be done; almost 900 ‘exercisers’ and ‘non exercisers’ shows no difference in either myopia progression or frequency of wearing glasses after follow up at 21 months.
Raman Gupta (below) investigated whether electronic displays could be a contributing factor to myopia development by measuring accommodation lag, stability and quality of vision under simulated monocular and binocular conditions. He and colleagues found that refractive state was less stable at closer distances, that all children exhibited accommodative lags at reading distances of 20-33cm and typical instant messaging text size is twice the size of the minimum text that could be resolved from their simulated displays, even in the presence of lag. This means that the eye has no reason to accommodate more to reduce lag as doing so would not noticeably increase image clarity – in other words, the eye, probably like many biological systems, is efficient (or lazy!). This work doesn’t prove that screens are a contributing factor to myopia development, but it does add knowledge that use of screens creates the type of optical environment, i.e. hyperopic defocus, suspected as being a stimulus for eye growth.
Of particular interest is that they found the accommodation response was less accurate at around 2-3D of stimulus than at higher or lower stimulus. As objects are brought closer (from a distance), the accommodation response becomes less accurate at around 50 to 33cm, but regains accuracy at distances closer than 33cm. It raises more questions!


About Kate
Dr Kate Gifford is a clinical optometrist, researcher, peer educator and professional leader from Brisbane, Australia, and a co-founder of Myopia Profile.

About Paul
Dr Paul Gifford is a research scientist and industry innovator based in Brisbane, Australia, and co-founder of Myopia Profile.












